[dropcap]T[/dropcap]HE JOINT CENTRE FOR BIOETHICS (JCB) at the University of Toronto does not shy away from a challenge. The centre was founded in 2002 with the mission of leading the charge in “bioethics research, education, practice and public engagement.” Two Canadian women, Gloria Taylor and Kay Carter, and their families recently provided the JCB and similar centres across Canada with an unprecedented ethical issue when they challenged the Attorney General of Canada for the legal right to physician-assisted deaths (PAD).
Carter v. Canada (Attorney General) became a turning point in Canadian law on February 6, 2015, when the Supreme Court of Canada ruled that the section of The Criminal Code that restricted physician-assisted dying deprived individuals of their charter right to life, liberty, and security of the person.
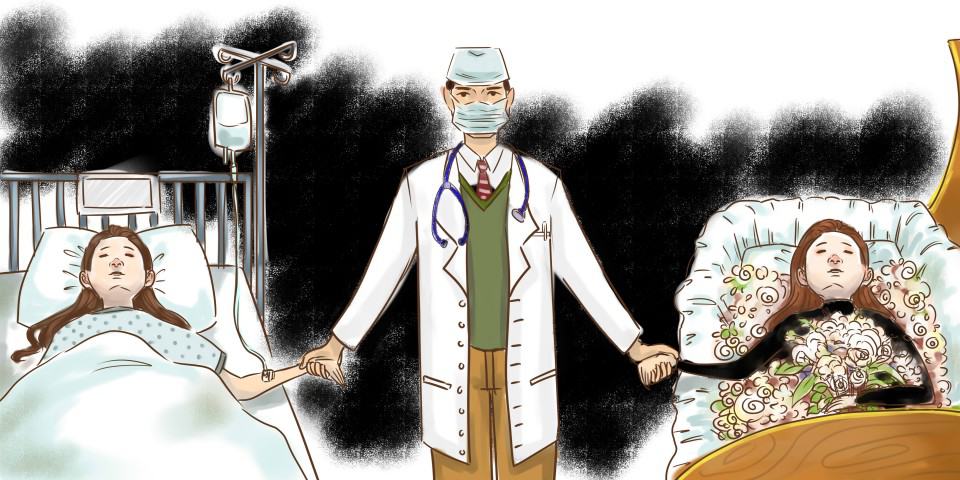
This ruling has major implications for the practice of medicine. It will no longer be a crime in Canada for a physician to honour the request of a “competent” person who asks for assistance in ending their life because of a “grievous and irremediable medical condition.” The judgement was suspended by the Supreme Court for one year, in order to give both federal and provincial jurisdictions — who will both be affected by this change — the opportunity to draft new legislation. This grace period has now been extended to June 2016. From now until then, patients can apply for an exemption to the Supreme Court’s suspension and be assessed for physician-assisted deaths.
While the Supreme Court’s decision detailed certain eligibility requirements for potential cases, many questions remain on how to move forward with this change, while still protecting the rights and freedoms of physicians and patients alike.
Legislators in Ontario continue to negotiate the complicated ethical implications of the Supreme Court ruling in an attempt to synthesize laws surrounding the practice. The University of Toronto, as an institution at the intersection of health research, policy, and practice, is a key player in this historic change.
Looking outward: the role of U of T in crafting PAD policy
Physician-assisted dying practices are in effect in many places around the world, including Oregon and Washington D.C. in the U.S., the Benelux countries, and Colombia. Québec crafted and implemented an assisted dying law on December 10, 2015, which resulted in Canada’s first legal physician-assisted death shortly thereafter. Last week, the first judicially authorized physician-assisted death took place in Calgary. The procedure was conducted by Dr. Ellen Wiebe, an advocate for PAD.
Pressure for the implementation of PAD in Canada has been rigorous and punctuated by passionate appeals from activists. Sue Rodriguez, a resident of Victoria, BC who suffered from ALS, became known as an activist for PAD in the early 1990s when she fought for her right to die. Despite having her case dismissed by the Supreme Court in 1993, Rodriguez died the following year with the assistance of an anonymous doctor in Victoria.
Other groups have opposed the change. The Council of Canadians with Disabilities has called for an “intervention” in the Carter case, arguing that PAD laws will normalize and legalize the harmful perception that death is preferable to disability.
It is within this complex and heated moral setting that Ontario and other Canadian jurisdictions must craft new legislation.
Trudo Lemmens, professor and Scholl chair in health law and policy at the Faculty of Law with cross-appointments at the Faculty of Medicine and the JCB, says that academics, and the University of Toronto in particular, have an important role to contribute to the debate.
“I feel it is our civic duty as academics working in relevant areas to [participate] in the debate and to help inform policy makers,” Lemmens said, adding that U of T professors have been active in making recommendations to government, participating as expert witnesses to the Carter case, and becoming involved in a variety of community groups.
Lemmens himself has been advocating for the development of a “strict regulatory regime with rigorously monitored safeguards” surrounding the practice of physician-assisted dying. On February 3, 2016, he gave a talk hosted by the Dalla Lana School of Public Health entitled Bioethics Seminar: Why Physician-Assisted Dying Can and Should Remain Restricted in Canada after Carter. This was one instance of an ongoing debate that has occurred at U of T surrounding PAD. “[W]e’ve had many more events at U of T on the topic in which I and other members of the academic community [participated] on different sides of the debate,” Lemmens said.
Another significant contribution to the conversation that U of T has made is through the formulation of interim recommendations to the many hospitals affiliated with the University of Toronto. The university is an integral member of the Toronto Academic Health Sciences Network (TAHSN), the only one of its kind in Canada, which institutionalizes collaboration between the university, its nine teaching hospitals, and four associate level members.
The JCB recently released a detailed list of key considerations for physicians dealing with PAD requests before the legislation comes into effect in June. The report was assembled by the Physician-Assisted Death Implementation Task Force, and it cautions physicians that are not currently compelled to perform PAD to focus on established ethical strategies and to seek legal advice, since the recommended process has not been previously tested. According to Lemmens, these recommendations will weigh highly with U of T’s many hospital affiliations.
Ethics of dying
In his seminar, Lemmens pointed to the development of PAD in Belgium as a fairly open and interpretive legislative regime. The criteria for PAD in Belgium include the following, as outlined in Lemmens’ memorandum on the topic for the parliament of Canada: “1. the patient is in medically hopeless situation; 2. of constant and unbearable physical or mental suffering; 3. that cannot be alleviated; and 4. resulting from a serious or incurable disorder; 5. caused by illness or accident.” This standard was brought into effect in Belgium in 2002.
Belgium has since seen an exponential increase in instances of physician-assisted deaths: from 347 cases in 2004 to 2,021 cases in 2015. One out of every 16 deaths in Flanders, Belgium can be attributed to PAD.
This is concerning for Lemmens, who noted that some language used in the Provincial-Territorial Expert Advisory Group on Physician-Assisted Dying Report mirrors that of Belgium’s and may not do enough to protect vulnerable people.
Vague criteria and terminology, Lemmens warned, could lead to premature deaths. He offered the example of a mandatory waiting period for PAD, which was not recommended in the advisory group’s report. Instead, this measure was recommended to be left to the discretion of physicians in collaboration with their patients.
“What me and other colleagues have said is most physicians will be responsible, but there [are] always, in any practice of medicine, there are sloppy people,” Lemmens said, emphasizing the importance of more stringent laws to mitigate the problem.
On the other hand, the Provincial-Territorial Expert Advisory Group, co-chaired by JCB director Dr. Jennifer Gibson, stated that the recommendations “place the patient at the centre” of the PAD process. This includes, according to the report, safeguards for vulnerable populations, including assessment by two physicians and robust assessment of eligibility, competence, and consent.
The future of health care
In October 2014, 84 per cent of Canadian respondents to an online poll agreed with the statement: “a doctor should be able to help someone end their life if the person is a competent adult who is terminally ill, suffering unbearably and repeatedly asks for assistance to die.”
This sentiment was echoed by some U of T students who are planning future careers in health care. For these students, the Carter case comes at a critical point in time. As some students see it, PAD will become an important aspect of ethical patient care during their careers.
“The patient has the right to control the time and means of his or her own death under the ethical principle of autonomy. Suicide is a legal act for theoretically everyone, but someone who is terminally ill or is disabled may not be able to exercise this option,” said Angela Han, a first-year medical student at U of T.
Joanna Dowdell, a U of T student who is also serving as a delegate for UN Health and Sustainable Development, agreed. “I think the introduction of physician-assisted [dying] in Canada is great. It ensures that people who would otherwise be forced to continue living in a lot of pain are now given another option, to end their lives when they want to, with dignity,” said Dowdell.
That said, Dowdell saw reason in Lemmens’ argument for a strict legislative regime surrounding the practice.
“I think there is definitely need for regulative body for oversight of the program, to ensure that [it is] not being misused and pushing vulnerable groups towards an unwanted procedure,” said Dowdell.
It is clear to see why protective measures are warranted. A new study forecasts that 74,000 patients will die of cancer this year alone, and many of those will not have access to palliative care in Canada. In fact, in spring 2014, the Canadian Hospice Care Association reported that only 16 per cent to 30 per cent of Canadians who die have access to palliative care. In this precarious situation, PAD risks becoming an alternative to other kinds of end-of-life care.
PAD must, therefore, be considered just one part of a much broader discussion of health care options. Han, for one, was not discouraged.
“[PAD] would not discourage good palliative care — the Netherlands and Oregon both became leaders in palliative care only after the medically assisted death was legalized there,” Han said.
Still, it is essential that policymakers, health care workers, and patients alike do not lose sight of holistic care in the ongoing discussions surrounding PAD.
In a 2015 study involving 100 patients suffering from a wide range of psychiatric disorders — such as mood, personality, post traumatic stress, eating, schizophrenia, addiction, autism, and complicated grief — who requested euthanasia, 38 of them withdrew their requests, and 11 others postponed upon being granted treatment.
In other words treatment is inextricably linked to requests for physician-assisted dying. Han and Dowdell, and many other students soon to enter health professions will have to navigate this fine balance.
Politics and pressure
As the June legislation deadline approaches, public feedback on PAD has grown increasingly heated.
Many religious institutions are voicing opposition to PAD as it becomes increasingly evident that it will become legal in Canada. Cardinal Thomas Collins of the Toronto Archdiocese made a statement against PAD in February.
A special Commons-Senate Committee, comprised of 11 MPs from the Conservative, Liberal, and NDP parties and five senators was struck at the beginning of January with the following mandate: “to review the report of the External Panel on Options for a Legislative Response to Carter v. Canada (Attorney General) and other recent relevant consultation activities and studies, to consult with Canadians, experts and stakeholders, and make recommendations on the framework of a federal response on physician-assisted dying that respects the Constitution, the Charter of Rights and Freedoms, and the priorities of Canadians.”
The committee of MPs and senators put forward 21 recommendations to the government on February 25.
Canadian students will be able to participate in discussions surrounding physician-assisted death over the coming months and as the practice is implemented. For Han, Dowdell, and many others, the policy will be a defining ethical consideration in their careers for years to come.