[dropcap]I[/dropcap] ate whenever, whatever, and however much I wanted to, and no one could stop me. For numerous reasons, I was always stressed and exhausted as a child, making food my ultimate coping mechanism.
During my time in high school, I would find myself staring at an empty family size bag of Doritos far too often during the week. I subsequently gained a lot of weight. By the age of 17, I was slipping into my second stage of obesity.
During that time, I found that society does not give these types of illnesses the authentication and accreditation they deserve, because they have an illusionary linkage to ‘vanity.’ Realistically, it is quite the opposite. Eating disorders are real mental illnesses, and the lack of legitimacy they receive needs to change.
Due to prolonged research and an outpouring of therapeutic effort, the tables have shifted towards acceptance of eating disorders as real issues — not entirely, but it is a humble start.
In August 2010, American Viewpoint conducted a national telephone survey of American adults for the National Eating Disorders Association. Eighty-two per cent of respondents believed eating disorders to be real physical and mental illnesses that should be treated; only 12 per cent of respondents believed them to be related to vanity.
However, if you have ever laid eyes on the magazine section at a cashier lane, the expectation of certain body parts looking a certain way in order to appear ‘beautiful’ is evident on their covers. Cosmopolitan’s May 2016 issue reads, “Flat Belly Fast! ZERO CRUNCHES.”
Eating disorders are not vanity, but they can be induced by body image insecurity. Unhappiness with a certain body type can even fuel binge eating disorder (BED), eventually exacerbating the situation. Contrary to popular portrayals of eating disorders, not all of them are centred on extreme weight loss.
As a child, I was bullied for my size, poked and prodded by people telling me to lose weight or else my health would decline. They would warn me — as if I didn’t know it myself — about feeling trapped in a body you did not wish to be in.
I did not aspire towards this lifestyle — I felt like I was thrown into it, with a complete loss of control. The pressures surrounding me made me feel as though food was an enemy, yet I couldn’t help but have this eerie and delusional love-hate relationship with it.
Although I am still learning the ropes of a healthy and active lifestyle, I have ceased to hate food and the act of eating, which has speeded my recovery process immensely. It took six years to realize I was tired of a way of life that I did not wish to be a part of anymore.
“I realized it was eat or die”
Rachel Ng, a second-year student at Ryerson University, also experienced life shackled to the restrictions of an eating disorder — anorexia nervosa. She became anorexic when she was nine but only got professional help seven years later. At 17, she went into cardiac arrest and required one and a half years of inpatient care to stabilize her health.
“Besides the obvious rules of eating everything I’m given in recovery, I had to replace a crumb if one fell on the floor, be supervised in the bathroom, and I wasn’t allowed to stand up without permission,” Ng said. “It was so hard that I ran away a few times and ended up getting a security guard to wheel me around in my wheelchair everywhere for a few months.”
Food choices also influence the way people feel about themselves. The Journal of American Dietetic Association reported, “81% of 10 year olds are afraid of being fat. 51% of 9 and 10 year old girls feel better about themselves if they are on a diet.” Ng’s story is an example of an eating disorder developing from a very young age.
“It was only until seven specialist doctors gave me the choice to enter hospice [end of life] care due to failing organs that I realized it was eat or die,” Ng said.
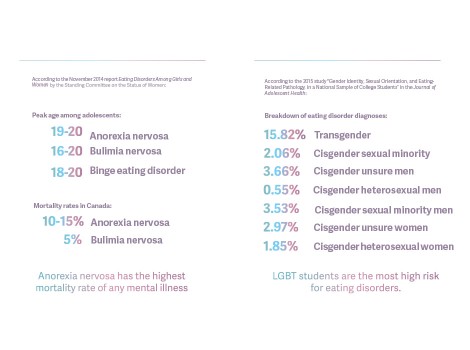
Like in Ng’s case, many eating disorders can prove to be nearly fatal, and anorexia nervosa is the third most common chronic illness among adolescents. This does not include the numerous reports and findings on BED and bulimia nervosa. Some people also exhibit signs of multiple eating disorders and do not fit into a single category.
According to Dr. Blake Woodside, psychiatrist, U of T professor, and director of Toronto General Hospital’s inpatient eating disorder program, those with anorexia nervosa are genetically predisposed to it. “Something has to happen to them to activate the genetic predisposition,” he explained. “An example is physical assault resulting in post-traumatic stress disorder acting as the activation.”
Most of the people he has encountered with eating disorders are those who have been abused sexually or physically. Eating disorders can also develop with other mental illnesses, like depression.
One first year student at UTSG, who prefers to remain anonymous, became depressed in grade 12 and had a low appetite. She decided she wanted to focus on getting healthy as her depression and anxiety got worse.
“When I realized this, I decided I wanted to actually use ‘losing weight’ as a distraction to the depression, and in my mind I figured, ‘If I focus on my body, the depression will feel less consuming, and at the same time I’ll lose weight finally!’” she said.
However, due to her depression, she became “reckless,” eventually testing low calorie levels of 500–800 per day. She joined an online forum of people with eating disorders for weight loss help. Although she never mentioned her eating disorder to anyone, her guidance counsellor eventually took notice.
“I tried to get better on my own instead and focused on another extreme diet with lots of fruits,” she said. “I figured it was better than starving but I still wasn’t going to eat like a normal person because at that point I was scared of a lot of foods. When I upped my intake, I started having lots of digestion problems, and my doctor gave me probiotics for that. Eventually I started gaining weight. At first I was horrified, but gradually I stopped focusing on that. The depression was getting better too.”
She added, “Even though I am better now. It still lingers in the back of my mind.”
In a similar way, I still struggle with the urge to raid my kitchen and leave my fridge completely empty, but I am better at maintaining control and knowing there are other activities I can use as an expressive outlet.
A plethora of disorders, no singular response
Eating disorders are not static or uniform and need to be talked about. They are not something we can throw a blanket response over and forget about; one individual’s eating disorder is never the same as another’s.
The experiences different people have dealt with can quite literally shape the activation and development of these illnesses. One of Woodside’s patients had four different types of depressions, and throughout that time, the patient had developed anorexia nervosa.
Woodside and his colleagues are working towards novel therapeutic techniques to aid those suffering with eating disorders. One of the five programs he described is called ‘Neuromodulation,’ which uses specific area techniques to rewire the brain to work in different ways.
“We are interested in this because there are many documented brain abnormalities with anorexia,” he said. “We try to use transcranial magnetization, which is non-seizure inducing. It stimulates a tiny part of the brain in the area responsible for processing feelings, bingeing, and purging.”
Also, Woodside and his colleagues are currently in the process of developing ‘Transcranial Magnetic Stimulation’ (TMS) specifically for bulimia nervosa; they are currently waiting to hear about a grant for their research before they get started. It would be for treatment resistant patients, and they would receive around 20–30 sections of the therapy, which is based on how the brain is wired.
Woodside explained that patients with bulimia nervosa are weight and shape preoccupied, addicted to dieting, and only binge as a result of being hungry. These individuals attempt to control or reduce the caloric impact of their consumption via induced vomiting, laxative intake, or exercise.
On the contrary, those with BED are unrestrained eaters and do not necessarily diet. Due to these differences, the treatment methods for each diverge significantly.
“Every body is different”
What exactly, is the fascination with weight and the way our bodies look? I still ask myself this question every day. Frustration bubbles inside of me as I realize that phrases like ‘I’m having a fat day’ are considered an acceptable topic of conversation.
Dr. Hilde Bruch, author of Eating Disorders: Obesity, Anorexia Nervosa, and the Person Within, wrote, “The obsession of the western world with slimness, the condemnation of any degree of overweight as undesirable and ugly, may well be considered a distortion of the social body concept, but it dominates present day living.”
We are expected to look aesthetically pleasing and fit a window of perfection that does not exist.
For example, a few years ago on Twitter, there was a viral tweet floating around that said, “If you weigh more than 200 pounds, please don’t wear leggings in public.”
Somelife published an article about this tweet and Bowling Green State University student Sara Petty, who took a stand against the fat shaming participants. They compiled a stream of her photos in which she took pictures of herself in each of the categories of clothing people were condemning someone of her weight for wearing. She conclusively tweeted, “Girls: Wear whatever the hell you want.”
Fat shaming is one cause for the influx of negative mentalities amongst those struggling with eating disorders. People like Sara reassure the world that we do not have to feel uncomfortable in our bodies. Instead, we should be able to live comfortably without the pressure of reaching unrealistic ideals.
The National Eating Disorders Association wrote, “It is important to remember that every body is different. We all have different genetic and cultural traits. Even if everyone started eating the same things and did the same amount of exercise for a whole year, we would not all look the same at the end of the year.”
When I was struggling with my BED, I truly wished to change but did not have the positivity or motivation to flip my life around. Not knowing how to escape a horrible habit like this is frightening. I reached out to family members and they supported the start of my weight loss and fitness journey.
Woodside said, “Families have a bad reputation with eating disorders since back in the 1980s. They are blamed for these illnesses, but they actually help the struggling family member get over the disorder — they don’t cause them. They are the greatest support. Families do not cause eating disorders. Period.”
There is strength in seeking help
As university students, our time is precious and it goes by fast. Taking the time to observe and understand your health will benefit you both mentally and physically. Understanding that not everyone speaks about or exhibits signs of their struggles may help create the solutions people with eating disorders need.
“It has been a year since I recovered psychologically and became weight restored, but I still see doctors once a week because I waited too long, so I encourage anyone with even the slightest bit of eating disordered tendencies or thoughts to get help right away,” Ng said.
Reaching out for help does not have to be difficult or frightening. Celebrity fitness trainer and weight loss coach Heidi Powell said in a blog post, “Seeking help may seem like a sign of weakness, but it is truly a sign of strength.” Connecting with others can help the healing process.
There are many facilities available not only at U of T but all across Ontario as well. For those battling eating disorders — take the first step and reach out for help. It may just prove to be the first raindrop in a storm of health benefits on the way to recovery. Eating disorders are real, deadly, and very scary, and no one should have to deal with them alone.