Researchers from U of T, in collaboration with scientists from Florida State University (FSU) and the Karlsruhe Institute of Technology (KIT), have discovered that enriching certain sizes of silica nanoparticles improves their ability to enter human cells, opening potential avenues for the design of drug delivery vehicles.
Nanoparticle drug delivery addresses one of the prevailing failures of the pharmaceutical industry: of the tens of thousands of drug candidates that the industry churns out each year, the vast majority fail. Many are too poorly soluble to enter the bloodstream, some flush straight through the kidneys, and others fall apart in the body before they can be of any benefit.
Scientists seeking to rescue these casualties of the drug discovery pipeline have turned to nanoparticles.
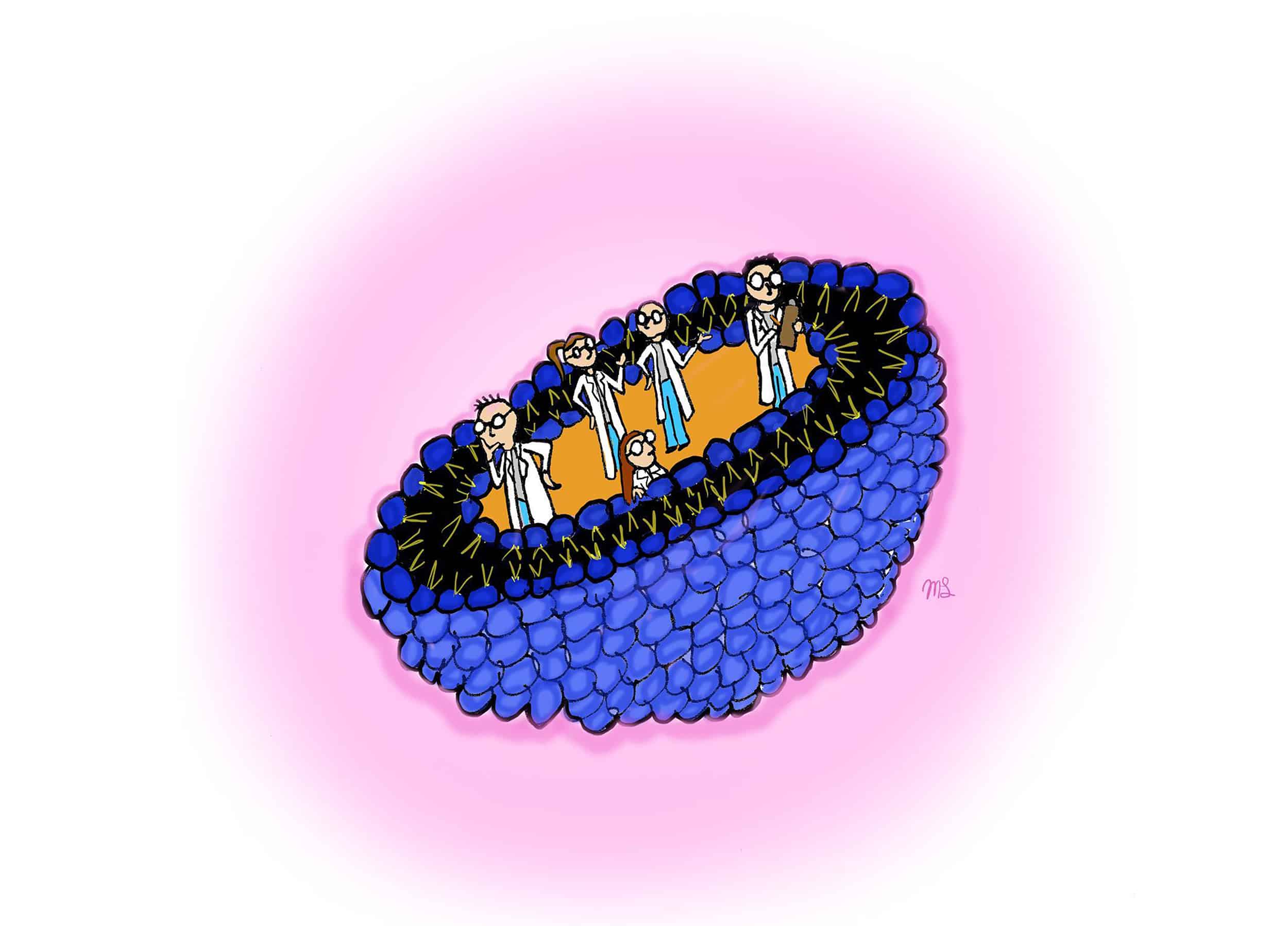
Nanoparticles measure millionths of a millimetre in diameter. Because they occupy the same size range as proteins, they accumulate inside cells by exploiting the cell’s existing mechanisms for engulfing biomolecules.
Drugs loaded within nanoparticles can thus hitch a ride into the cell interior. Nanoparticles also protect drugs, hiding fragile molecules from the physiological environment and screening hydrophobic, or ‘water-fearing,’ molecules from the watery interiors of our bodies.
As always, when we meddle with our cells, we can do harm as well as good. Particles of the wrong material, or the right material in the wrong size, can induce cytotoxicity, damaging the cell’s lipid membrane and causing oxidative stress, or genotoxicity, which harms the genetic information that encodes the cell.
Scientists seek to maximize the benefits while minimizing the harm. For that, a deeper understanding of nanoparticle toxicity is required.
The Florida-Toronto-Karlsruhe team leapt to fill the knowledge gap. Led by Dr. Steven Lenhert from FSU, Dr. Geoffrey Ozin from U of T, and Dr. Christian Kübel from KIT, they measured the cellular toxicity of various sizes of silica nanoparticles.
Better known in its macroscale forms as sand or quartz, silica is relatively cheap and chemically inert. It forms nanoparticles that were “previously reported to be less toxic comparing to other semiconductor nanoparticles,” according to Chenxi Qian, a PhD student in Ozin’s lab. “That’s why we are more interested in them.”
They are also demonstrably effective. In laboratory dissolution studies, silica nanoparticles enhance the dissolution rate of poorly soluble drugs, and in beagle dogs, they increase bioavailability — the percentage of drug that reaches the bloodstream after ingestion.
But less toxic is not necessarily non-toxic, and even silica is not without potential drawbacks. As demonstrated in some laboratory studies, it has produced inflammation and causes oxidative damage in cells.
The researchers sought to better understand this toxicity and how it may be driven by particle size. They treated a lab-bred cell line using lipid-coated silica particles of varying diameters and found that some size ranges depressed cell viability significantly more than others.
Then came a twist: contrary to the current understanding of nanoparticle toxicity — that smaller particles tend to be more toxic, possibly due to their larger surface area-to-volume ratio — diameter of the particles did not correlate with toxicity.
Equally interesting was when the team measured the toxicity of a sample of pooled nanoparticles, which contained particles of all sizes, and found it to be relatively low, even though some of those sizes exhibited higher toxicity when used alone. In the nanoparticle production process, chemists first produce a single batch comprised of many particle sizes and then separate the batch into different-sized fractions. During that separation process, the research team postulated that they must have enriched some fractions for toxic factors.
The team hypothesized two possible drivers behind these more toxic fractions. First, that certain fractions might be inherently more toxic; second, that all sizes of nanoparticles might be equally toxic, but the more toxic fractions might more readily enter cells.
The team found little evidence to support the first hypothesis, but when they tested the second, they saw the more toxic nanoparticles at a higher intracellular density. Under a fluorescent microscope, the more toxic fractions lit up the cell interiors.
This discovery reveals a contradiction in the functioning of our vehicles of drug delivery: we want them to enter cells to deposit their cargo and produce a therapeutic effect, but it is precisely this easy entrance into the cell that seems to increase their toxicity.
Any attempt to reconcile these opposing effects will require a better understanding of how nanoparticles interact with cells, especially with the cell membrane, the most obvious barrier to entry. At the end of their paper, which was published in Nature Scientific Reports, the team laid out their next steps: to further delve into the toxic fractions, enrich them for their most active components, and elucidate their mechanisms of interaction.
The tools for safer, more effective drug delivery lie tantalizingly on the horizon. In their recent work, Lenhert, Ozin, and Kübel have taken us closer. We will walk the next mile, but first come more experiments.