Tackling long wait times by committing to consistent follow-ups
I am always told by well-meaning friends, colleagues, and strangers on the internet that I should never be scared to reach out for mental health support. Yet when I try to make a counseling appointment at UTM’s Health & Counselling Centre (HCC), I am told that the next available appointment is a nearly month away. Adept at masking the urgency of the issue, I don’t push for an earlier appointment. By the time I meet my counselor, the event triggering my mental illness has passed and my feelings have somewhat subsided because I have already indulged in the unhealthy and self-destructive coping mechanisms that I was hoping to avoid. I leave many of my counseling appointments feeling like they are a waste of time and thinking that I don’t need to go back.
Months go by between my counseling appointments, meaning that any feelings that arise between sessions usually don’t come up by the time my next appointment comes around. The HCC, well aware of my precarious mental health given the extensive phone survey I had to fill out before I began counseling, never follows up with me during these months. This simply enables me to continue putting off counseling appointments because there is no one to hold me responsible, causing my mental health to worsen. It is a vicious cycle: I cannot attend counseling because my mental health is too poor, and my mental health remains poor because I do not attend counseling.
U of T’s mental health services, despite being available, are not actually accessible. Long waiting times and lack of follow-up between counseling appointments are detrimental to students seeking help for their mental illness. They allow students to indulge in unhealthy coping mechanisms without any intervention. The university needs to address this problem by implementing policies to ensure that counselors continuously keep in contact with all students who report mental illness, and that the number of counselors available for students is proportional to the student population on campus.
Zeahaa Rehman is a third-year student at UTM studying Linguistics and Professional Writing and Communication.
Revising the university’s action plans to make them less show, more substance
Students’ limited access to the mental health resources available on campus is reflective of a dearth of information and resources about treatment. Millennials experience higher levels of mental illness, with suicide being the second leading cause of death for young people in Canada. Although broader initiatives are being pursued to destigmatize mental illness and support mental health, these are not the best means to treat specific ailments — students often require access to specialized services.
The university offers relatively little information on how to access mental health aids on campus, and much of what is offered can be unclear. While U of T’s main mental health website shares its vision and initiatives for making treatment of mental health on campus a priority, the heightened grandeur presented about what the university can offer to someone experiencing a mental health crisis comes off more like useless jargon rather than a constructive path to a healthier mind.
In my own experience of needing help and reaching out, I simply did not know how to put together a plan of action given the information I was presented with online. This lack of useful information presented an obstruction that discouraged me from seeking further resources beyond the website, which ultimately worsened my depression and anxiety.
There are many complexities associated with establishing a better mental health framework. However, this issue is one that requires a simple solution. When someone is feeling distressed, they need to be given information and resources in the clearest way possible. Posting convoluted reports online for the sake of keeping up appearances is not useful to addressing individual experiences and does not provide sufficient guidance at a time where guidance is very much needed.
Rehana Mushtaq is a second-year student at Innis College studying English and Religion.
Directing funds to address shortages in professionals on and off campus
The biggest problem with the mental health system at U of T is that there simply aren’t enough therapists to keep up with demand. We’re among the largest universities in Canada, but somehow we don’t have enough doctors to service students — which is unacceptable.
According to The Globe and Mail, a fifth of Canadian postsecondary students suffer from some kind of mental illness, such as depression or anxiety. If we were to transpose this figure to U of T’s 70,000-person undergraduate population, that would mean over 14,000 students need to be able to access adequate mental health care. Unfortunately, many are going without.
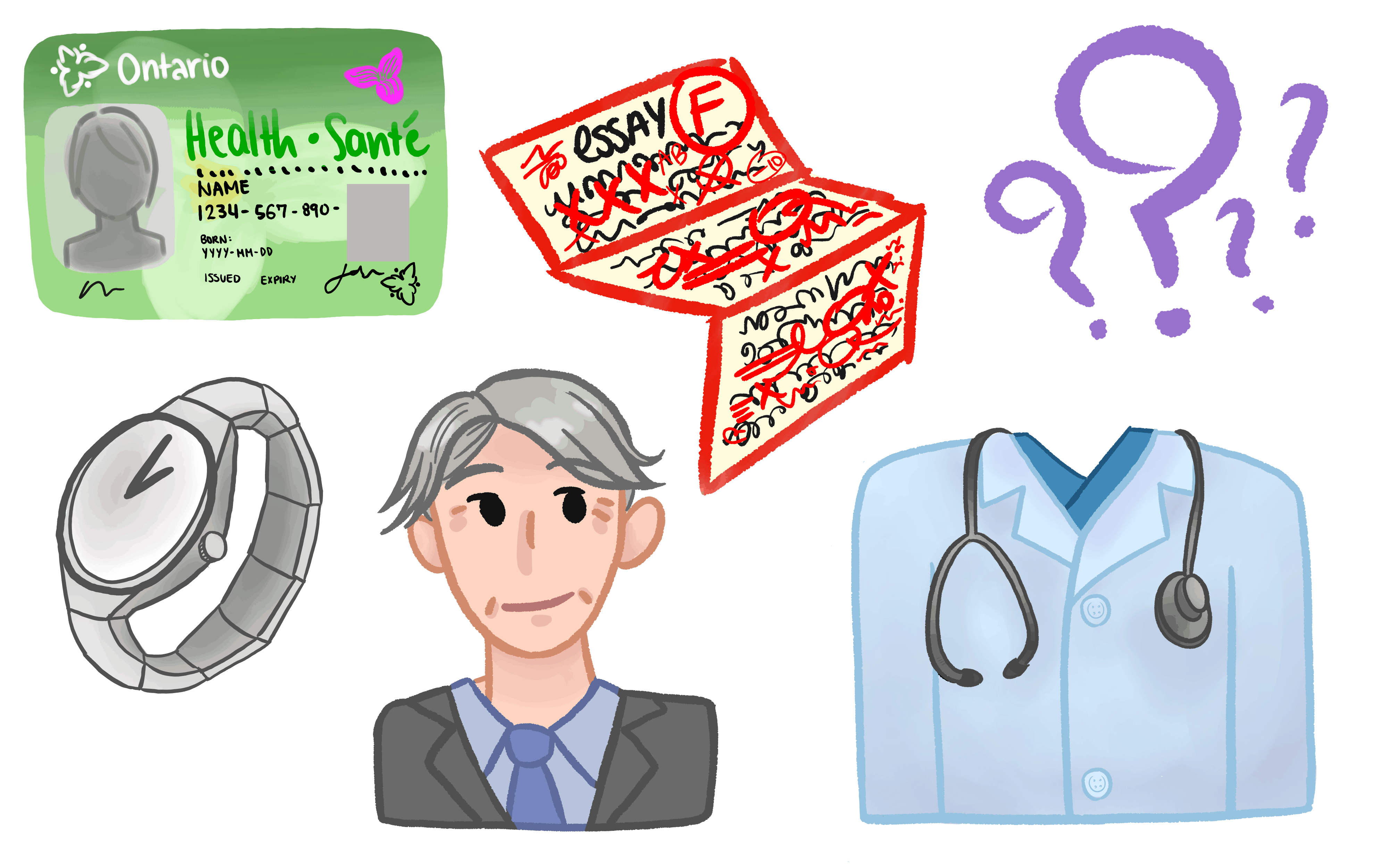
I’m one of them. I’ve been able to access a general practitioner at U of T who prescribed me an antidepressant to help with my anxiety, as I don’t have a family doctor. However, I have been trying since October to speak to a therapist in the U of T system, with no luck whatsoever.
Now, if U of T doesn’t want to be on the hook for failing to supply therapy to the students who need it — especially given the stress that takes place within the university itself — the least they could do is improve student health care coverage so we can see people outside the system. Student Life’s website claims that the University Health Insurance Plan (UHIP) may include “counselling and psychological services,” but these services aren’t listed on UHIP’s website or in its information booklet. Studentcare, the supplementary health insurance plan offered by the University of Toronto Students’ Union, does cover some psychological counseling services — up to $125 per visit, and a maximum of 20 visits per policy year — but they will not cover psychotherapy, which is often more expensive.
Either U of T needs to hire more counselors and beef up their mental health care for students, or students should be provided with the resources to help them see people outside the university.
Adina Heisler is a third-year student at University College studying Women and Gender Studies and English. She is The Varsity’s Student Life Columnist.
Removing counterproductive limits on counseling sessions
There is no time limit on healing. But U of T’s strategy for addressing and supporting mental health is flawed; by limiting quantity of care, it also limits students’ ability to recover.
Upon experiencing a traumatic event and being diagnosed with post-traumatic stress disorder, I sought a solution through the UTSC Health & Wellness Centre. Although everyone I encountered throughout my experience was extremely kind and understanding, I was faced with harsh university policies on mental health and wellness. Namely, I was informed that the university’s health insurance plan only covers the first eight sessions of therapy.
For a university with such an outstanding reputation and track record, I was shocked that I would be thrown into my recovery journey on an agenda. No one can easily accept their situation, open up and trust in a professional, and heal on a calendar timeline. It took me almost six months to build up the strength to tell a professional what I had been through. I have no doubt that the therapist would be just as supportive as everyone else in the office, but it is extremely distressing to think that I would be kicked to the curb after my eighth session.
The important fact to take away here is that there is no uniform healing process. I concluded that I would rather pay additional money to my tuition and bills in order to fund additional sessions off campus, rather than try and prematurely work through the thoughts that accompany trauma. I cannot imagine how frustrating this information is for someone whose condition is more paralyzing than mine, including students who cannot afford mental health therapy outside of U of T.
Amarra Mohamed is a second-year student at UTSC studying Journalism.
Eliminating the need for family doctor referrals
The Health & Wellness Centre at UTSG offers services for mental health like group therapy, individual psychotherapy, and pharmacotherapy. There isn’t much in the way of procedure listed on the Health & Wellness website, but after trying to find out about the assistance that is available, it became evident that getting help isn’t as straightforward as the website makes it seem.
Before any assistance is offered, the Health & Wellness Centre requires a family doctor’s referral and consent to gain access to past medical records. Though the referral can be done through a doctor external to the university or through one of Health & Wellness’ staff, no alternatives to this process are offered, and the folks at reception insist on new patients getting this referral. Upon calling the centre later and asking for justification, they said that this is just the way the system works, and without it, the procedure to get an appointment would take much longer. After pressing for options that don’t require this referral process, I was rerouted to the various embedded counseling options that are run by upper-year students at U of T’s colleges, faculties, and departments.
Getting a family doctor’s referral isn’t always possible, nor is it what people necessarily want to do, given, for instance, a potential lack of comfort in confiding one’s mental health issues to a general practitioner. The Health & Wellness Centre should look at treatment options that don’t require intermediary steps such as this one. Drop-in services and appointments throughout the day would enable students to talk to someone who is licensed and who has the ability to help them in some capacity. Going from these brief appointments to a more serious care plan would be a good next step — and while this step may require a referral, there should be options to continue with care for patients who aren’t able to provide one.
Aimin Shahid is a second-year student at Victoria College studying English and Writing and Rhetoric.
Encouraging professors to be understanding and flexible
Speaking both from personal experience and the testimonials of others, students still find it difficult to admit to their instructors that their schoolwork is suffering due to illnesses that aren’t immediately ‘visible.’ Simply arriving to class late or failing to meet the deadline for an assignment, even with advance notice, might be greeted with hostility or outright refusal to accommodate. It is the responsibility of everyone in the classroom to create an environment more conducive to talking about mental illness. Nevertheless, many professors will often express how precariously exhausting undergraduate life is, but they aren’t willing to change the practices in their classrooms that might make things worse.
This isn’t just a problem at U of T. At Carnegie Mellon University, a renowned centre of educational reform strategies, anthropologist Lauren Herckis found that sticking to a familiar style of lecturing is often a higher priority for instructors than implementing needed changes to their teaching style. Professors are at the top of their fields, and it is understandable that they might find it hard to relate to students’ problems. But changes to specific practices can also spur positive developments in mindset.
For example, professors should be open to deviating from rigid timeframes. U of T can and should be the first to experiment with new training for teachers — similar to existing diversity training — geared toward mental illness and accessibility. Just as colleges have counselors on hand, perhaps we should consider assigning more counselors to faculties, so that students can talk to someone with knowledge of the coursework with which they are struggling. If we can’t expand the reach that Accessibility Services can cover, then perhaps we should be telling professors to trust the word of a student more than they do now. The reality is that no student wants to fall behind or let their schoolwork suffer — so when it happens, they often have good reasons.
Arjun Kaul is a fourth-year student at St. Michael’s College studying Neuroscience.
Making essential changes to classroom pedagogy
If the university wants to improve mental health, then it should also look to the classroom. Given the stress that academics often create in students’ lives, we can and must transform how we teach, learn, and assess.
For starters, professors should eliminate late penalties for assignments. Fear of mark deductions only induces stress and anxiety, and it does nothing to enhance our learning. These penalties should be forgotten and replaced. Instead, deadlines should be negotiated, fairly staggered, or automatically extended.
The way participation marks are calculated should also be revisited. Participation marks often do little to assess our understanding or committment to course material. Instead, they deduct arbitrary marks from those who find themselves unable to go to class or too anxious to speak in front of a crowd. Participation can be measured in more accomodating ways, such as written reflections or short online quizzes.
Finally, we should also allow students to negotiate syllabuses with professors at the beginning and even throughout the term. Given the diversity of skills in the classroom, students ought to have some influence over their preferred assignment styles — for instance, opt for written work instead of presentations. Instructors can also offer students options as to how to distribute the weight of assignments, alongside flexible deadlines. Such measures are not unprecedented in courses at U of T.
Some other suggestions include having ‘do-over’ policies, expanding credit/no credit options, having mandatory professor check-ins and feedback sessions, uploading lectures online, and having instructors set up study groups for large classes.
Changes like this would transform university pedagogy as we know it. Instructors should be motivated to adapt curricula to accommodate students’ needs and desires in order to prevent the learning process from being a drain on our health and well-being.
Stanley Treivus is a fifth-year student at Innis College studying Human Geography and Political Science.