A new tumour analysis technique has been created to tackle the most common type of pancreatic cancer, in a new U of T-affiliated study. This method could improve physicians’ ability to better predict how a patient will be affected by the cancer, as well as reduce the health care costs of this type of analysis.
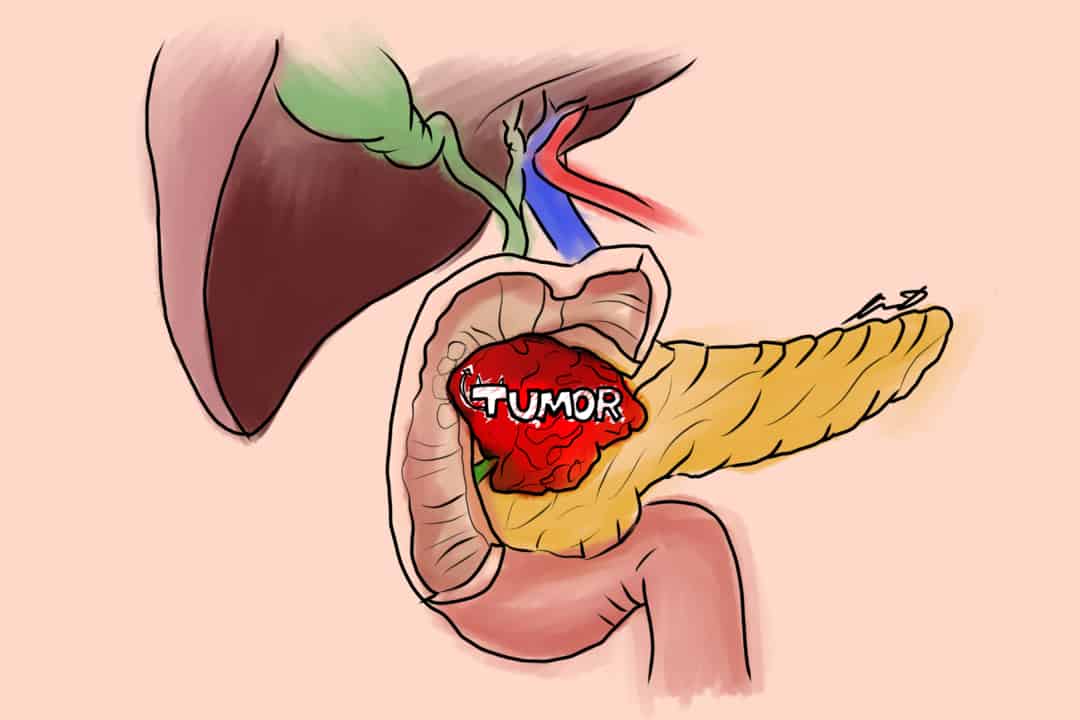
The researchers investigated pancreatic ductal adenocarcinoma (PDAC), which is the fourth leading cause of cancer-related deaths in the world. It is predicted by scientists that PDAC could become the second leading cause of death by cancer by 2030.
The current system for analyzing tumours is flawed
Physicians currently use a three-tiered grading system to analyze tumours from PDAC. The system relies on the classification of tumours into three groups: well, moderate, and poorly differentiated.
The best tumours for pathological analysis are well differentiated, while the worst are poorly differentiated, according to Dr. Sangeetha Kalimuthu, an Assistant Professor at U of T’s Department of Laboratory Medicine & Pathobiology, in an interview with The Varsity.
Tumours in the middle of the scale are considered moderately differentiated. “Think of a well-formed ice cream,” she continued. “When it starts to melt, it gets all ugly and not really pretty to look at, so that’s in essence how a tumour behaves.
But a major problem with this current grading system is that most tumours from PDAC are identified as moderately differentiated. Tumours with this classification are of limited clinical utility, explained Kalimuthu, as they provide little useful prognostic information about the patient.
Recently, large–scale studies have identified prognostically significant molecular subtypes in PDAC. Different subtypes of PDAC are associated with differing clinical outcomes.
However, direct identification of a patient’s molecular subtype of PDAC through molecular analysis is expensive and not readily available worldwide.
New study offers cost-effective solution for overcoming limitation
The U of T-affiliated study, co-authored by Kalimuthu, identified specific structural — or morphological — patterns in PDAC tumours and presented a novel tumour classification system based on these patterns.
The new classification system presented in the paper correlates morphological patterns with the known subtypes of PDAC. This enabled physicians to identify the molecular subtype of PDAC without using costly molecular analysis.
Kalimuthu added that looking at tissue stains “is the standard bread and butter of pathology.”
“Taking a tiny piece of tissue that you get from a much larger tumour and sequencing it doesn’t give you a representation of the tumour,” she said.
“We look at these stains so we can actually get an idea of the tumour — nothing [such as other techniques like sequencing] gives you a better picture of [it].”
Future potential to integrate technique with artificial intelligence
An established procedure that provides precedent for this newly developed classification system for PDAC tumours is an existing grading system for prostate cancer tumours.
Researchers devised the system, called Gleason grading, in 1966. It similarly gave prognostic information for colon cancer patients.
Kalimuthu and her co-authors hope that their new tumour grading system can fulfill a similar role for PDAC.
In the future, Kalimuthu and her co-authors hope to validate the PDAC-based grading system with a larger cohort of pathologists, before incorporating the grading system into a clinical setting.
If they can achieve this, the improved system of prognosis could help guide physicians in developing treatment plans for patients with PDAC.
Since the new classification system is based on patterns, Kalimuthu believes it could one day be integrated with artificial intelligence.
“This classification system could be directly applicable with deep learning algorithms — so that’s the long-term goal.”