On January 23, 1922, a 14-year-old boy who was severely ill at the Toronto General Hospital became the first person to receive a purified insulin shot. That boy was Leonard Thompson, and like many others, he suffered from diabetes.
According to the World Health Organization (WHO), about 422 million people in the world lived with diabetes in 2014. The number didn’t decline as the decade went by: more recent data from the International Diabetes Federation show about 537 million people with diabetes as of 2021.
Although these statistics are disconcerting, it is perhaps of consolation to remember that while diabetes was once considered a fatal disease, now, with the discovery and distribution of insulin, people with diabetes can lead normal lives. It is not an overstatement to say that insulin, Frederick Banting and Charles Best’s discovery at the University of Toronto, has saved millions.
What is diabetes?
Simply put, diabetes is a chronic disease where glucose, the body’s and brain’s main fuel, cannot get into the body’s cells. Glucose comes from the food we eat or is produced by our bodies and enters the bloodstream during the digestive process. Once there, the pancreas detects the rising glucose levels in the bloodstream and releases a hormone called insulin. Insulin works like a key, opening a unique door in cell membranes so glucose can leave the bloodstream and access the cells.
The effect is simple: glucose levels in the bloodstream decrease, and your cells will have fuel to work so your body can perform its duties, such as thinking, breathing, and moving every single muscle of your body. Yes, that includes every beat of your heart.
Now, if the insulin hormone, which plays a pivotal role in the process of glucose cellular uptake, fails to do its job, there are consequences. Depending on the reason for insulin failing to fulfill its role, people contract different types of diabetes.
“It’s not me. It’s the pancreas”: this is the case in type 1 diabetes. Here, the pancreas — the sole organ responsible for producing and releasing insulin — produces little to no insulin, meaning that patients within this group depend on external insulin to live. This is the type that Leonard had, and it tends to appear in childhood and teenage years. Type 1 diabetes primarily stems from an auto-immune response — whose exact nature remains unknown — that affects the pancreas function.
“It is still not me. It’s the pancreas and the cells”: this is the case of type 2 diabetes. Here, either the pancreas produces little to no insulin, or cells don’t respond to the insulin, which is also called insulin resistance. In the latter scenario, the body’s cells don’t recognize insulin as a key, and therefore, glucose won’t be able to cross the cells’ membrane. This results in overwork from the pancreas as it tries to lower rising glucose levels, a vicious cycle that can lead to the organ’s own failure. This type is mainly seen in adults because it is triggered by life factors such as diet, lack of physical activity, age, and metabolic conditions.
There are other types of diabetes which are mostly associated with very specific conditions. For example, gestational diabetes occurs during pregnancy in women who weren’t diagnosed with diabetes before. If treated correctly, the condition will reverse after childbirth; if not, there may be severe and life-threatening consequences for the fetus.
What happens if insulin doesn’t do its job?
Our body cells interact with specific molecules via “mediators.” Insulin is one of these mediators. It arrives at the cell membrane and triggers a cascade of events that transports the glucose through the membrane, as cells won’t interact directly with glucose due to the glucose’s size and molecular complexity. So, if the insulin doesn’t help the glucose get into the cell, glucose will keep flowing in the bloodstream.
A high glucose level in the blood is called hyperglycemia, and it can become dangerous for various reasons. Firstly, glucose is sticky. Similar to when you overload your coffee with sugar so that the drink becomes thicker, glucose will make blood more viscous and sticky. The more glucose is present in the blood, the more likely the big molecule will adhere to the membranes of the tissues it encounters while travelling through the bloodstream.
In particular, glucose will eventually adhere in the eyes, causing blindness; the kidneys, ending in renal failure; the heart, causing strokes and heart attacks; the vascular system, causing clogged veins and atherosclerosis; and the nerves, leading to a loss of mobility, especially in feet and legs. Combined with damage to the vascular system, diabetes-caused damage to the nerves can end in amputations. The overall consequence of untreated diabetes is a progressive organ failure that is not compatible with life.
Secondly, and most importantly, hyperglycemia’s persistence over time can lead to what an untreated diabetic patient will experience as symptoms of diabetes. Although not all individuals are the same and, therefore, experience different things, initially, it is most likely that hyperglycemia will increase the rate at which a person urinates; tons of glucose in the blood require the kidneys to work harder to filter it out of the blood via urine. The more you urinate, the more water you need to drink, so uncontrollable thirst is another symptom of diabetes.
In addition, someone with hyperglycemia might feel extreme tiredness and experience weight loss. Although there is tons of glucose in the bloodstream, insulin is not there to help it get inside the cells. When the cells are not receiving fuel, they will send signals to the brain for you to eat, eat, and eat.
Under this panorama, a person with these symptoms might feel irritated and have intense headaches, including blurred vision. If the hyperglycemic state remains uncontrolled over time, it will lead to organ damage and progressive organ dysfunction.
The gift of insulin, the medicine
Today, over a hundred years after that early morning when Banting woke up to draft a 25-word hypothesis to cure diabetes on a piece of paper, insulin is one of the best medicines we can use to control hyperglycemia.
The administration of external insulin into the body is a resource used by millions of people with diabetes every day. Nowadays, multiple devices are available that help people with diabetes sense their glucose levels and better dose an insulin shot.
Insulin, as medicine, is vital for patients with type 1 diabetes, where their pancreas produces insufficient insulin. This contrasts with type 2 patients, where adequate care and diet can leave an insulin shot as a last resort. In fact, an early diagnosis of type 2, in a stage called pre-diabetes, an accurate treatment design from physicians and dietitians that patients adhere to can result in the ability to avoid insulin therapy altogether.
The science and technology applied to research over the years since insulin’s discovery have helped to make better diagnoses and treatments. Challenges for people with diabetes today include accessibility to insulin as a medicine, a need for better delivery methods for the drug administration to improve life quality, and lastly, an overall social change regarding diet, physical activity, stress management and work/life balance.
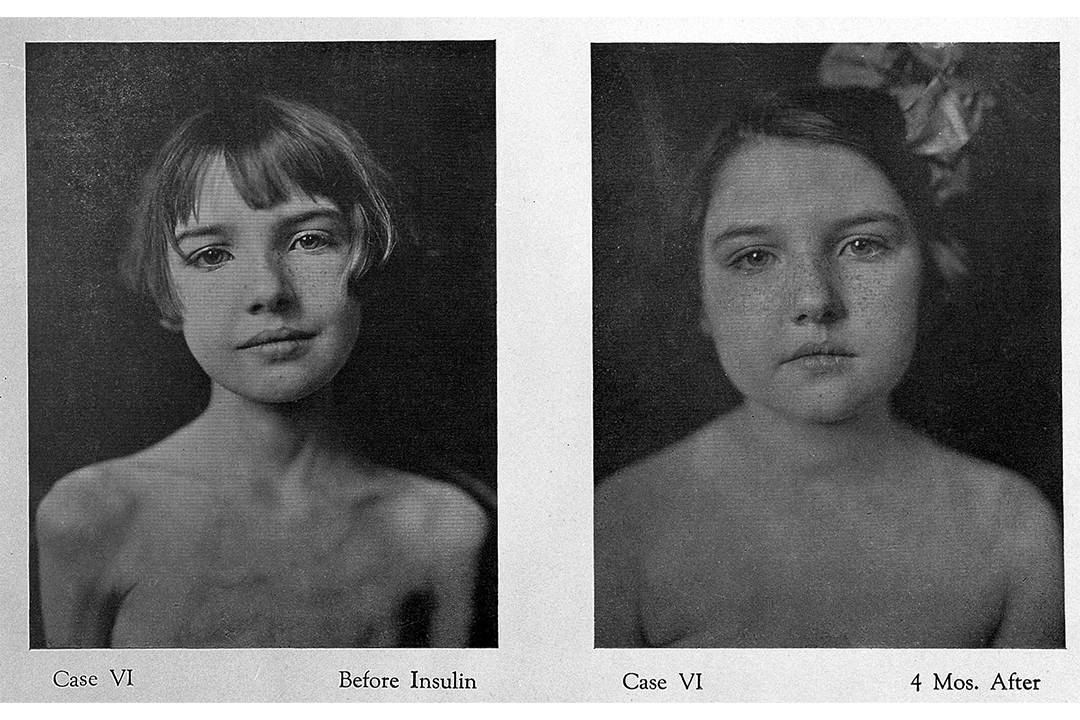
The effect of Banting and Best’s discovery at U of T is powerful. Imagine Leonard Thompson coming in and out of unconsciousness and receiving the first purified insulin shot, showing signs of improved health and subsequently going on to live. This was a miraculous outcome.
A U of T surgeon described patients with diabetes after taking insulin as being “awakened dramatically, snatched from death’s door.” This is all thanks to the endeavours of Banting, Best, J. J. R. Macleod — an international expert in diabetes who pushed Banting to pursue his idea — and James B. Collip, who helped purify the extract, making it safe for human trials. What a riveting story of collaboration and creativity, based here, at U of T.