Endometriosis is a reproductive disease that affects 10–15 per cent of women of reproductive age and is associated with significant prolonged psychological stress in social and sexual situations.
But it’s also much more than just a medical condition. Endometriosis is a disease with a long history of sexism and scientific disinvestment. Understanding the condition requires a historical lens into how institutional and cultural forces hinder reproductive care for women and gender minorities.
What is endometriosis?
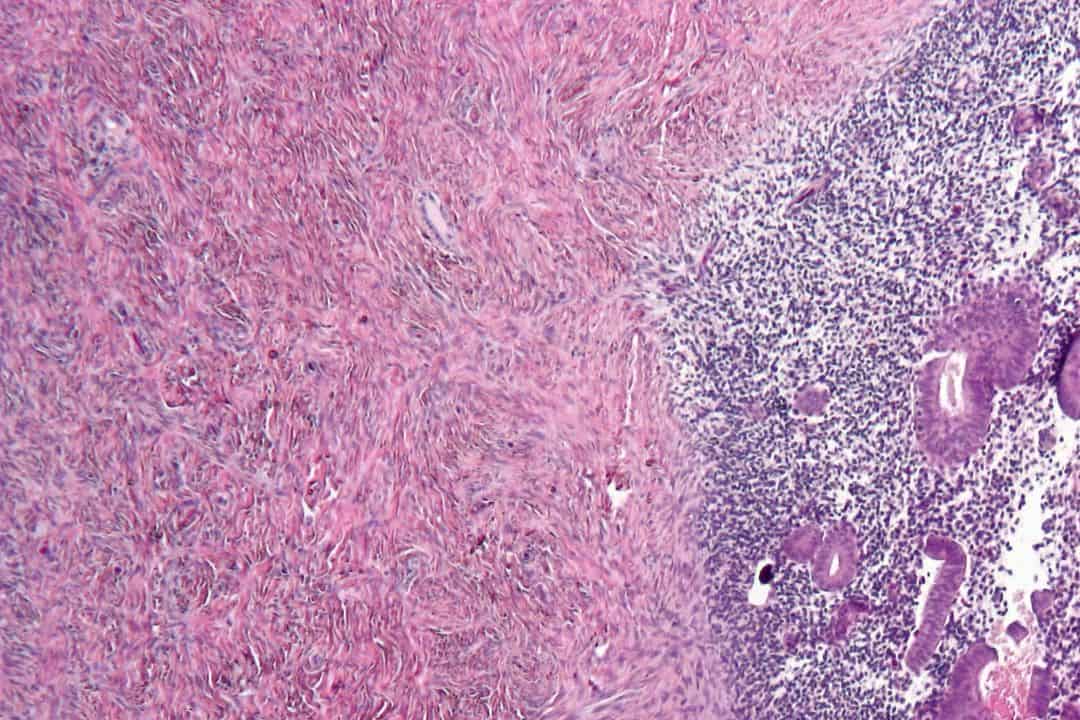
The endometrium is the inner lining of the uterus, which, during monthly menstruation, thickens and sheds as a response to hormonal changes. In endometriosis, the endometrial tissue grows outside of the uterus — on the bladder, ovaries, and fallopian tubes — resulting in the formation of scar tissue and inflammation.
Endometrial tissue that grows outside of the uterus still responds to hormones that cause thickening and shedding, but due to its abnormal location, the shedding cannot be discharged by the body, and instead, accumulates in the abdomen.
When endometrial tissue grows in inappropriate places, it develops into cysts and scar tissue that compromise the overall function of affected pelvic organs. Consequently, endometriosis results in different challenges including hormonal imbalances, sexual dysfunction, severe pelvic pain, infertility, and psychosocial issues.
Difficulties with diagnosis and treatment
Though endometriosis affects a significant portion of the population, scientists and doctors lack effective diagnostic measures and treatments. Many patients begin experiencing symptoms of this disease in adolescence but struggle to receive adequate attention and individualized treatment from their healthcare providers — in fact, there the average delay in diagnosing endometriosis across ten countries is 6.7 years after the initial symptoms set in, according to a 2011 study by Kelechi E. Nnoaham and colleagues.
Biomarkers are measurable substances and signs in the body that may indicate someone’s predisposition to developing a disease or illness. Scientists speculate that biomarkers, genetic vulnerability, dietary patterns, and retrograde menstruation — the flowback of menstrual blood into the fallopian tubes — may predict the deposition of endometrial cells outside of uterine lining. While these may contribute to endometriosis, according to an article in Current Obstetrics and Gynecology Reports, the evidence linking them to the development of endometriosis is inconclusive or scarce.
The struggle to understand the causes of endometriosis manifests through its invasive, faulty, and painful diagnostic procedures and treatments. For example, to be diagnosed with endometriosis, patients must endure tests that rule out other causes of pelvic pain and subsequently undergo biopsies and surgical procedures to confirm to treat endometrial tissue abnormalities.
Even when individuals are diagnosed, the lack of knowledge about endometriosis shrouds the path to treatment in mystery. As of yet, there is no cure for this disease, meaning many women go through several trial-and-error treatment options that are more rooted in managing severe and excruciating pelvic pain than treating endometriosis.
Why is endometriosis a medical mystery?
We cannot understand the medical difficulties with endometriosis in a vacuum. Gynecology has historically erased and trivialized women’s experiences with pain, leading to misdiagnosis or improper treatment plans. This historical erasure also allows for stigma and misinformation to proliferate about women’s and female reproductive health.
The neglect of endometriosis originates from a strong gender bias in medicine where cisgender men are used as the standard model for health and disease. Conversely, women are treated as the ‘other,’ and infantilized in the knowledge and experience of their own body. This reality is changing, but progress is slow.
Endometriosis’ ambiguous status, lending to a lack of cure or sufficient knowledge about its pathophysiology, has generated misinformation and deepened oppressive stereotypes that harm many women’s self-image and resiliency. For example, a common myth since the ’70s was that endometriosis only affected women who bore children later in life, leading many to associate endometriosis as a ‘career woman’s’ disease.
An article published in The New York Times describes medical gaslighting as “the experience of having one’s concerns dismissed by a medical provider.” It also contextualizes the reality of endometriosis. Despite growing interest, the lack of medical knowledge about the precise workings of endometriosis is often colloquially discussed as an inherent property of the disease rather than resulting from the systemic neglect of research into women’s health.
Ignoring pelvic pain is a common way misogyny manifests in healthcare and continues to hinder scientific and social progress. Gendered expectations to be sacrificial or submissive discourage women to be vocal about the physical and psychological pain of endometriosis. Even if women express their pain, they are frequently branded as overtly emotional by their doctors, constituting a form of erasure and preventing women from accessing the right care.
This ignorance also halts progress in the field: doctors and researchers not taking into account women’s experiences of pain can seriously reduce the accuracy of classification systems and formal definitions used for diagnosis.
Self-silencing in endometriosis
For patients with endometriosis, the misunderstanding, neglect, and systemic failures they endure to properly diagnose and treat endometriosis can strain their mental health, ability to cope, and relationships with themselves and others.
Unsurprisingly, the culture of diminishing womens’ pain and self-silencing is connected to a fragmented sense of self: a 2020 Feminism & Psychology study about how experiences with endometriosis affects self-perception found that when women silence themselves or belittle their pain to maintain amicable relationships, they often experience a loss of their sense of self.
Endometriosis is a public health concern with a history of misogyny and oppression that backlogs scientific progress and endangers womens’ health. When doctors, scientists, and even loved ones ignore or misunderstand women’s pain, it goes toward not only erasing the pain, but also the well-being of women who endure it.


No comments to display.