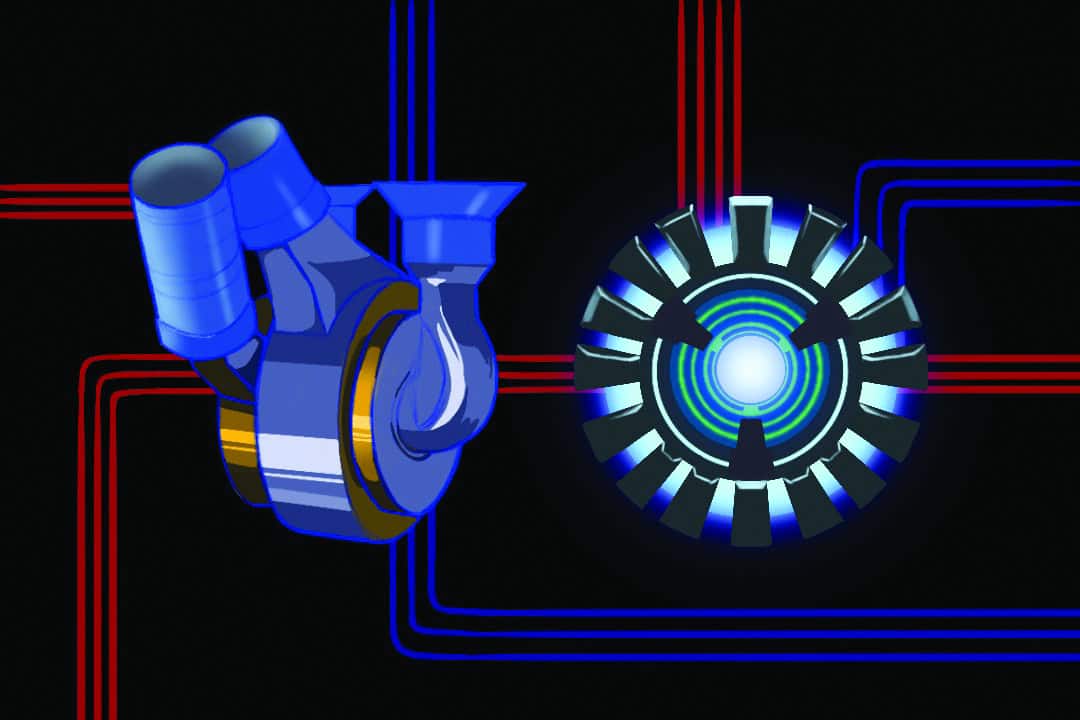
Marvel fans are familiar with the story of Tony Stark and his artificial heart — the “arc reactor” — which allowed him to survive after experiencing a life-threatening heart injury. Until now, artificial organs at this level of function were just a fictional concept.
Biomedical scientists at BiVACOR, a US-based medical device company, have made the concept a reality by developing the Total Artificial Heart (TAH) which can revolutionize medical treatment for patients dealing with heart failure. This artificial heart may not be as flashy as Tony Stark’s or come with Iron Man’s suits, but it aims to save the lives of patients with severe heart failure — much like the arc reactor.
Although in its early stages of in-human implantation, the TAH has already saved two lives and, with continued success, it has the potential to become a viable alternative to traditional heart transplants.
What is heart failure?
Heart failure is a condition in which the muscles of the heart cannot pump enough volumes of blood to meet the body’s demand for blood and oxygen. The human heart has four chambers, two of which are the left and right ventricles that pump blood out of the heart and into the rest of the body. Heart failure can affect the left, right, and sometimes even both ventricles. Biventricular heart failure occurs when both the left and right ventricles of the heart are affected.
Heart failure affects at least 26 million people worldwide and the Heart and Stroke Foundation estimates that up to 750,000 Canadians live with heart failure, and 100,000 are diagnosed each year. Heart transplants are reserved for patients with severe heart failure, for whom drug therapy is limited and would be relatively ineffective compared to a transplant. However, with only approximately 6,000 donor hearts globally available each year, many patients who need a transplant cannot receive a donor heart.
Revolutionizing artificial heart therapy
BiVACOR is a company specializing in designing medical devices and is currently in its clinical stages, meaning its products are being tested on humans in a clinical setting. The company’s founder Daniel Timms is credited for inventing the TAH. His journey in creating this revolutionary medical device began with applying his biomedical engineering knowledge while working with his plumber father to experiment with constructing devices similar to heart valves using water pumps.
BiVACOR aims to demonstrate the TAH’s commercial application and viability to encourage additional investments. These investments would be used for the TAH’s full commercialization, so that patients who require a heart transplant will no longer need to wait years for a potential donor. As of December 2023, 3,428 Canadians were waiting to receive a heart transplant.
With the commercialization of TAHs, patients will have access to them and can improve their quality of life much faster.
How does the TAH work?
BiVACOR’s TAH is a biventricular blood pump providing blood to both the systemic — or full body — and pulmonary — lung-specific — circulations. It’s designed to be a long-term replacement for a recipient’s heart, mainly for patients with end-stage biventricular heart failure: the most severe form of heart failure that can only be treated with transplants or implanted assist devices.
For patients with severe univentricular heart failure — ventricle failure of only one valve — the TAH may only be used in specific cases where a left ventricular assist device is not a recommended form of treatment. The TAH can also act as a short-term heart replacement for a patient on a transplant waiting list.
The TAH combines a centrifugal rotary pump to transport fluids and magnetic levitation, which holds items in space using opposing magnetic poles to suspend a rotor — the part that spins — between the two pumping chambers to propel blood through both of the circulatory pathways. Unlike a heart, the TAH requires no valves, contracting ventricle chambers, or a diaphragm. It comes with an external controller and rechargeable battery system for untethered operation.
The TAH is small, compact, and suitable for the bodies of most men and women. Despite the small size of the TAH, it’s capable of pumping blood at 12 litres of blood per minute, which is enough blood flow for an adult man undergoing strenuous exercise.
The first concern that may come to mind with a mechanical heart is the possibility of metal corrosion. However, the TAH is constructed from titanium which is compatible with biological materials such as human bodies, corrosion resistance, and strength.
Successful in-human implantations
On July 9, BiVACOR conducted its first FDA-approved in-human implantation of the TAH at the Texas Heart Institute on a 57-year-old patient who was a man on a waiting list for a heart transplant with end-stage heart failure. The patient had the TAH for a total of eight days, after which a donor heart was made available.
A few weeks later, a second implantation was performed at the Duke University Hospital. The 34 year-old-patient, Donavon Harbison, experienced biventricular heart failure and was grateful for the new life with the TAH. Harbinson went on to say, “I’m like, OK, I am going to be Tony Stark… I’m about to come out with a shiny piece in my chest that keeps me alive.”
With restored circulation, the TAH allowed Harbison to regain enough strength within 10 days to also undergo a heart transplant and receive a donor’s heart. Both implantations demonstrated the TAH’s aforementioned short-term use as a “bridge-to-transplant” solution.
Looking to the future: Where science meets sci-fi
An artificial heart may just be the beginning. Even though currently the TAH has been used as a stop-gap for patients waiting for a heart transplant, it opened many possibilities. Imagine a future in which other organs — especially those most prone to developing illnesses — can be replaced with artificial versions. Although certain organs such as the brain are too complex to be replaced, other organs such as the bladder, stomach, and lungs, may be replaceable with artificial implants like the TAH.
While reading about the TAH, I couldn’t help but make a connection to the many sci-fi novels, films, and series that depict human cyborgs, and how this breakthrough may be one of the many steps that lead to something similar to that concept. Some may view this advancement and become worried, whereas others may yearn for such a future. Is it possible that we may see humans undergo cybernetic enhancements or cosmetics in the form of mechanical integrations? Only time will tell.
In the meantime, we should all welcome and embrace any such invention that helps save or improve lives, whether the invention is of natural or mechanical origin.


No comments to display.