It was Frederick Banting’s co-discovery of how to extract insulin in the early 1920s at U of T that continues to save millions of lives across the globe, providing hope to patients suffering from diabetes who, in previous years, had none.
For Dr. Sue Tsai and Dr. Dan Winer at the University Health Network (UHN), insulin is the gift that keeps on giving.
“In [our] field a lot of people are looking at how obesity causes inflammation,” said Tsai. “But no one really knows it affects the immune system when it comes to infectious diseases, or cancer, because so many things are altered [and] your hormones are all dysregulated.”
Insulin’s role in diabetes is well-researched, but little is known about the role it has in regulating T cell function and what leads T cells to stop responding to insulin.
Tsai wanted to determine what factors cause obese individuals to have a reduced response to vaccinations, develop more infections, and be more likely to develop cancer.
They narrowed their target to insulin, because individuals become resistant to it when they become obese.
Tsai, a postdoctoral fellow at UHN, and Winer, an Assistant Professor in U of T’s Department of Laboratory Medicine and Pathology, have uncovered an insulin signalling pathway that elicits a response from infection-fighting T cells when they are activated.
Insulin, a pancreatic hormone, promotes glucose uptake via downstream signalling pathways. These pathways involve the binding of the insulin hormone to an insulin receptor (INSR).
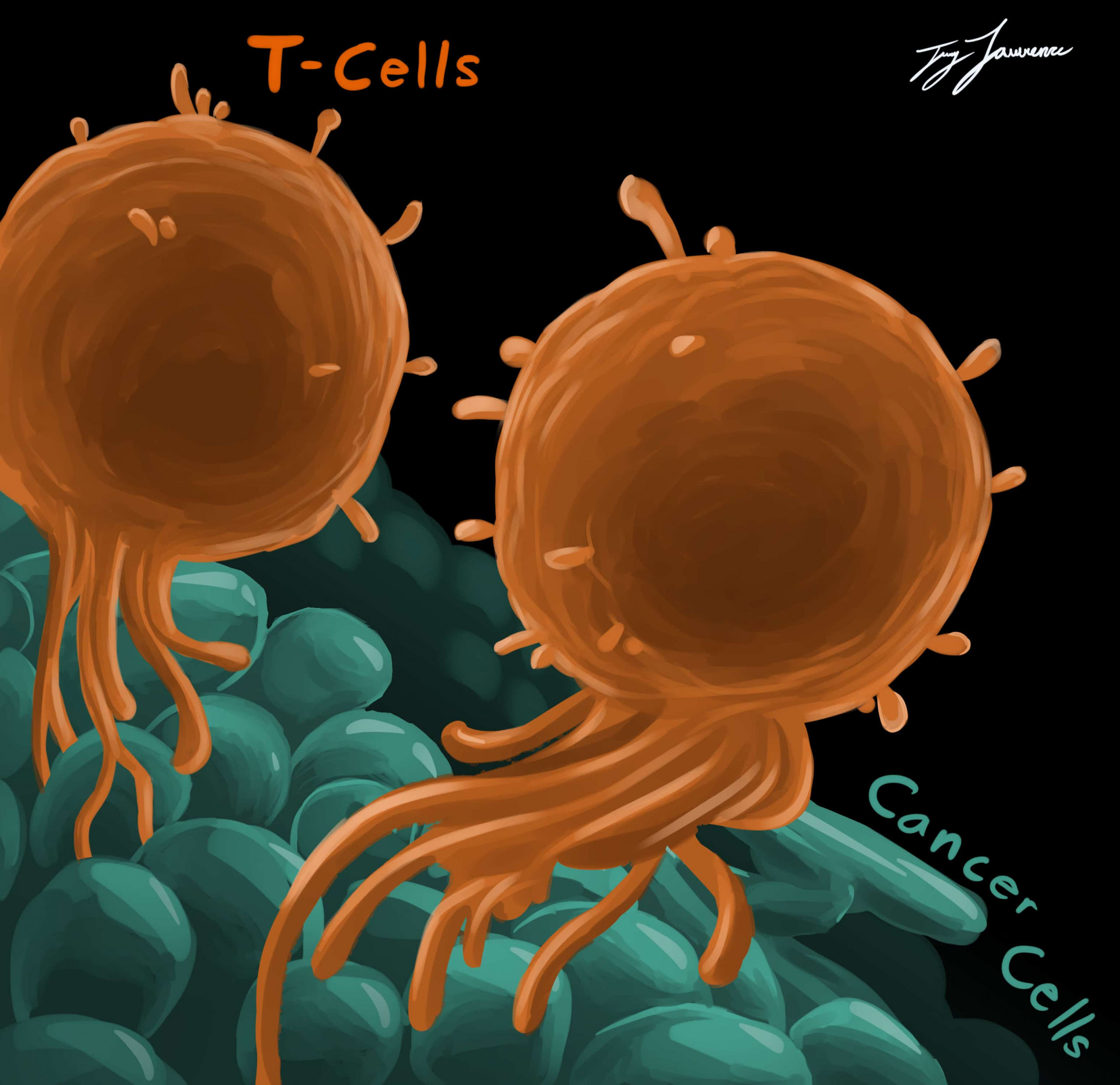
Immune cells, such as B cells and T cells, that protect the body against infection also possess this receptor. Tsai and Winer hypothesized that the binding of this receptor would stimulate T cell activation and proliferation, leading to a strong and immediate immune response.
In their study, Tsai and her colleagues compared T cell function in mice without the INSR to those with the receptor.
“We found that T cells [without INSR] become less functional, and when we give the mice influenza [H1N1], they do worse,” explained Tsai. “They lose more weight and then they have a weaker immune response against the influenza.”
INSR played an integral role in maximizing the potential function of the T cells in mice by increasing their nutrient uptake and in turn generating energy through ATP production during inflammation and infection.
The researchers’ findings provide some reasoning as to why vaccines in obese individuals may not be as effective. Many obese individuals are insulin-resistant and, as shown in this study, could therefore have a weaker T cell response.
T cells are integral to the efficacy of a vaccine, as they recruit infection-fighting antibodies and aid in immunological memory.
Tsai hopes to continue exploring the link between insulin and immunity, and is currently investigating insulin signalling in B cells. She believes the findings of these studies could have wide-ranging applications.
“The most obvious thing is influenza vaccines. How can we develop a vaccine, and what additional signals can we add to the vaccine to get them to work better in individuals who are insulin resistant?” said Tsai.
“Also, tumour immunotherapies. Do obese people respond to these therapies differently than non-obese people and does insulin resistance play a role in that?”
In the future, the insulin signaling pathway could also be used to study and find ways to ‘boost’ the immune system and develop vaccines that would work more effectively in obese individuals.
Tsai’s findings were published in Cell Metabolism last month, almost a century after the discovery of insulin.