Our genes contain strands of DNA that give us our distinguishing features. Some of these genes may also carry diseases and ailments that can affect our daily lives. But what if there were a way to remove those genes?
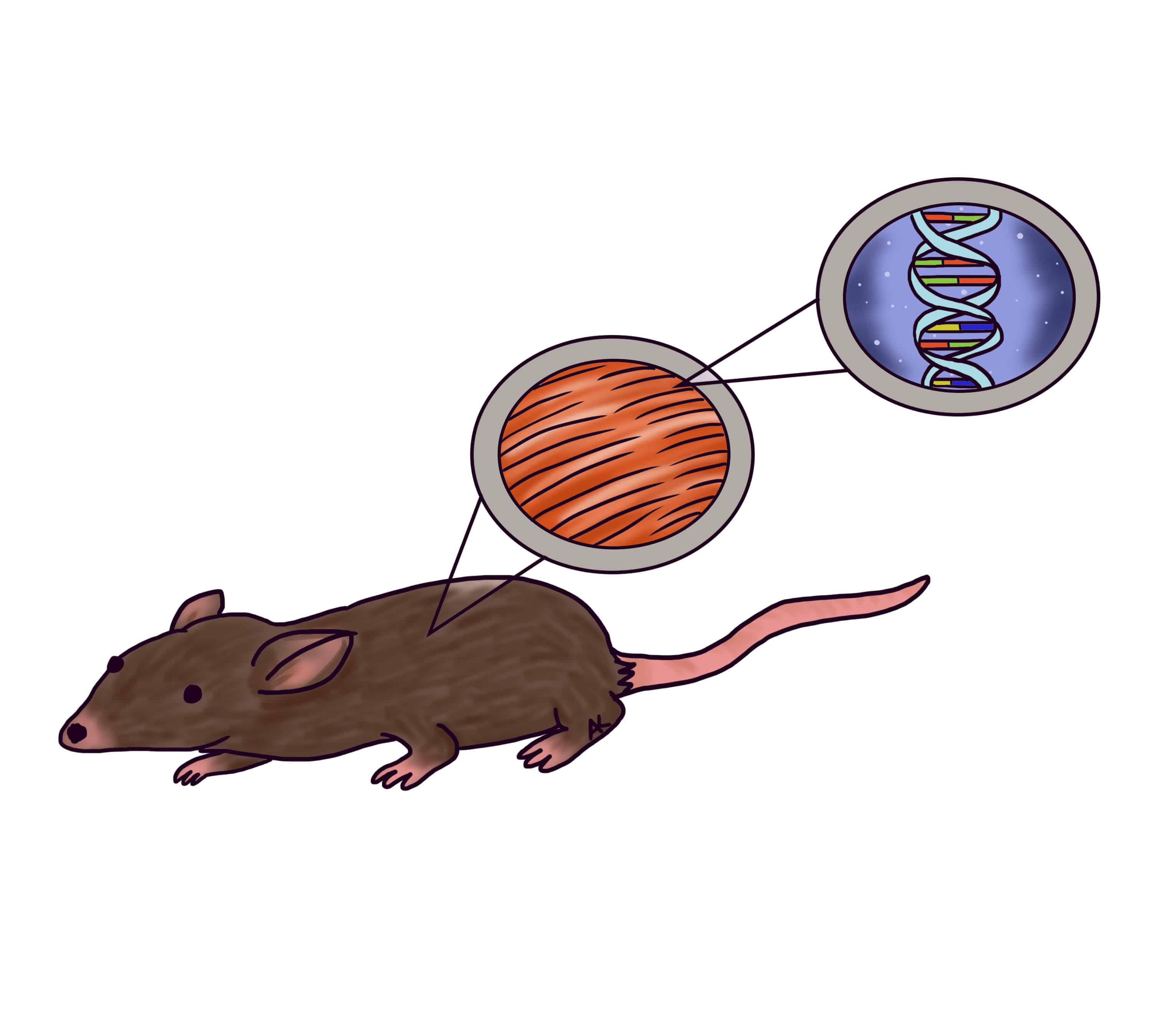
Scientists at The Hospital for Sick Children (SickKids) have used a gene editing technology known as CRISPR to snip out a gene that causes muscular dystrophy in mice. The study, recently published in Nature Medicine, was led by Dr. Ronald Cohn, the study’s principal investigator and Senior Scientist at the SickKids Research Institute.
The mouse model they studied had a form of congenital muscular dystrophy called MDC1A. This condition renders the body unable to produce dystrophin, a protein in muscle fibres that acts like a shock absorber. Insufficient function of these proteins will cause muscles to become a fat-like substance.
When infants are diagnosed with the disease, they will lose muscle function over time and eventually become paralyzed. People with this disease have a life expectancy of roughly 20 years.
In the study, the team restored muscle function in the mice by using CRISPR technology to ‘fix’ the disease-causing mutation classified as a “splice site mutation.”
CRISPR, which stands for “Clustered Regularly Interspaced Short Palindromic Repeats,” is a unique sequence of DNA in bacteria and other microorganisms that contributes to their defense against foreign genetic elements. CRISPR is useful for gene editing because it uses RNA to direct an enzyme called Cas9, which acts like molecular scissors to cut strands of DNA.
The research used the CRISPR system to cut DNA associated with skeletal muscles and peripheral nerves to improve the mice’s mobility. Focusing on these targeted areas has helped centralize the treatment.
“This is important because the development of therapeutic strategies for muscular dystrophies have largely focused on improving the muscle conditions,” said Dwi Kemaladewi, a Research Fellow at SickKids, in an interview with The Scientist. “Experts know the peripheral nerves are important, but the skeletal muscles have been perceived as the main culprit in MDC1A and have traditionally been the focus of treatment options.”
Cohn’s team used an efficient technique that allowed them to snip the DNA without having to replace it with a new piece of DNA. Once the CRISPR system cuts out the disease-causing gene, natural cell repair mechanisms can directly reconnect the severed strands of DNA so the sequence can be read normally. In some follow-up tests, it was observed that the mice regained a level of activity that was close to the control group of the non-affected mice.
CRISPR technology can be revolutionary for treating other muscle diseases like Duchenne muscular dystrophy (DMD), which Cohn’s team had worked on in 2015 in an effort to remove a duplicated gene and restore protein function in a patient. It also has the potential to treat other splice site mutations like congenital epilepsy and hereditary vision loss.
However, this technology has a ways to go before it can be used as a therapy for humans. A concern that researchers have raised is the unpredictability of how the body’s immune system would react to the bacteria used to produce proteins that the body cannot generate. Scientists are also unsure if CRISPR could cause other mutations in our DNA.
Using CRISPR to treat humans with muscular dystrophy may end up being ineffective because mature muscle cells in adults cannot divide, and so their DNA repair technology do not have the tools to add or correct genes. However, Cohn’s team is attempting to change this by working with nonreproductive “somatic cells” that have specialized into different cells.
Humans are more complex creatures than mice, and editing human genes may have unknown effects on future generations.
The future of CRISPR is bright, but the scientific community should use this tool with caution because it is still a very new technology. In an article in the Toronto Star, Cohn noted that it was unlikely for long-term patients with muscular dystrophy to recover muscle function. “Having said that, after speaking with so many patients and their families, if we can just keep them where they are and not have them deteriorate… that would already change the world for these patients,” Cohn explained.