“Do no harm.”
Upon entering the medical profession, nearly every physician takes some form of a medical oath. While the infamous phrase ‘do no harm’ does not hail from the original Hippocratic Oath, it heavily aligns with today’s core tenets of medical ethics: autonomy, justice, non-maleficence, and beneficence. Every day, we trust medical professionals to uphold these principles and treat patients to the best of their ability. After all, they took an oath.
But oaths can be broken. The integrity of the medical profession endures a continuous struggle between an empathetic responsibility to benefit the collective and the intellectual desire for answers and heroism, no matter the cost. As we unearth medical stories from the past, we also unearth some of the misdeeds committed in the name of science throughout history due to physicians’ and researchers’ failure to balance compassion with scientific inquiry. Among these misdeeds is the Tuskegee syphilis study.
The Tuskegee syphilis study
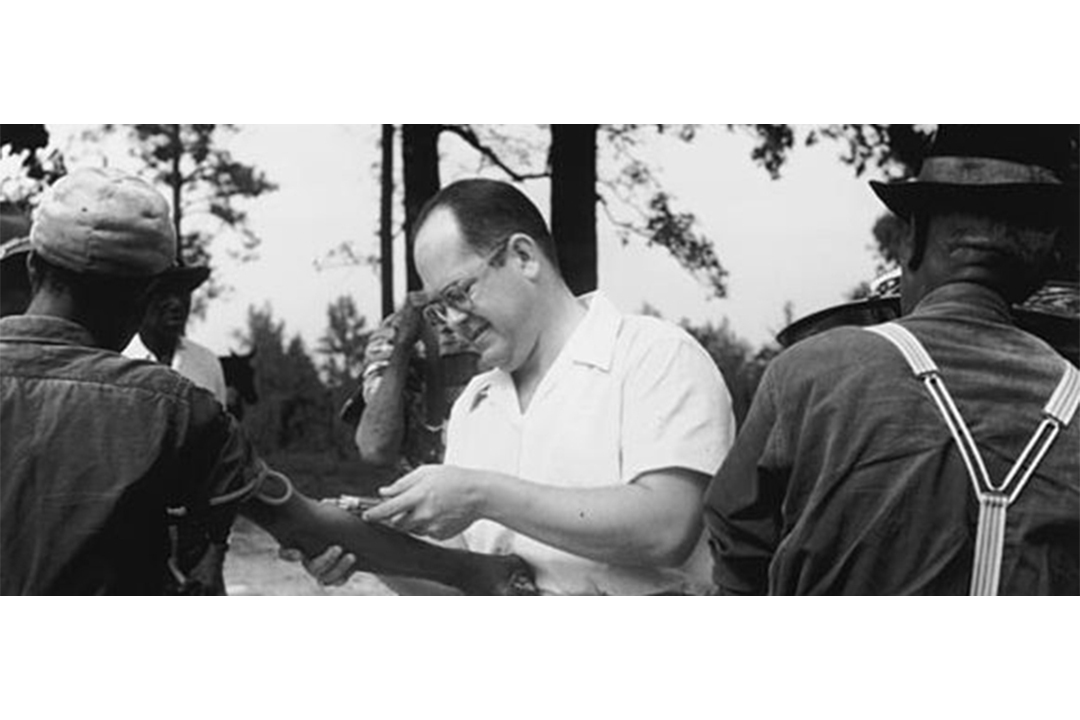
During 1932, the United States Public Health Service (USPHS) came to study the effects of late-stage syphilis in 400 African-American men in Tuskegee, Alabama.
The Tuskegee study was conducted when Social Darwinism — the idea that certain people gain power and influence in society because they are innately better than others — was extremely prevalent, particularly in scientific circles. As a result, efforts to corroborate the belief that there were fundamental differences between people of different races, and thereby to provide justification for discrimination towards people of colour, were enthusiastically welcomed by the scientific community. Researchers of the Tuskegee study used prevalent ideas like Social Darwinism to justify racial discrimination in their research.
Meanwhile, many Black Tuskegee residents welcomed the researchers with open arms because they had been misinformed about the purpose of the study. And so the USPHS doctors, spinning tales about life-saving research, felt further justified by the community’s misled support. What followed over the next several decades managed to violate the sworn Hippocratic principles of non-maleficence and beneficence beyond reproach.
Syphilis — despite being transmitted primarily through sexual activity — can have more far-reaching effects throughout the body, including cardiac and neurological complications. The antibiotic penicillin is currently used to treat many different types of bacterial infections, including syphilis.
Because the study aimed to examine the long-term effects of the disease, the doctors refused to treat the men even after the advent of penicillin in the 1940s, which became widely available in the 1950s. Some doctors even attempted to suppress the publication of papers about penicillin. Instead, USPHS doctors left the bacteria to fester for decades and watched, unmoved, as the men succumbed to the disease and died.
Even worse, the USPHS doctors didn’t inform the men that they had been diagnosed with syphilis. Doctors lured those who already knew of their ailment into the study with promises of a free cure. They were promised treatment, but time and time again, the doctors would only run tests on them and monitor them under the guise of curing them.
The men in the infected group of the study, believing that they were cured, or altogether unaware of their diagnosis, spread the disease to others. But the study continued all the way until 1972, after which an investigation by an advisory panel appointed by the Assistant Secretary for Health and Scientific Affairs concluded that the study was “unethically justified” and subsequently terminated it. Informed consent in human participatory research became defined and required by the US federal government in 1981. This public outcry against the Tuskegee study helped influence this regulatory legislation.
The ripple effects of the Tuskegee study on research legislation
In our current society, in which researchers are ethically required to inform patients about the study they are participating in and any associated risks, this type of deception seems unthinkable. Moreover, when some deception is required to carry out a study, researchers today are also mandated to debrief the participants afterward so that they understand what has been done.
The flaws of the Tuskegee study run deeper than the researchers’ dishonesty with participants — the study’s experimental design itself is dubious. Longitudinal studies, like the Tuskegee study, often have variables that can be difficult to control, as the circumstances of study participants can change vastly over the years in which the study takes place. The experiment, poorly designed and not adequately planned, swapped participants back and forth between the control group and the infected group due to some participants becoming infected and others being treated by outside doctors. Not only was this morally questionable, but it also rendered the study scientifically invalid.
Decisions between the desire for knowledge and the ethical implications of obtaining that knowledge are not always simple. By studying the disease and its progression, the USPHS doctors might have believed that their research would eventually save many lives — despite the harm caused to the 400 men in the infected group, which was unnecessary given the penicillin that was already available to treat them. The USPHS doctors evidently decided that, for them, this was a tradeoff worth committing to, even if it was made without disclosing to the participants that they were being sacrificed for the doctors’ own curiosity.
However, medical professionals today would likely disagree. Perhaps this difference in perspective results from far more robust ethical standards in scientific research. Regulations that take into account the participants’ willingness, such as informed consent and better transparency, are often required. Our standards for ethical research are progressing with the advent of an improved ideological revolution in how we approach topics such as privacy, personal autonomy, and racial and gender inequalities.
Among all of these competing considerations, unfortunately, the core purpose of the medical profession is sometimes obscured. At its core, medicine should not aim to push political agendas or satisfy intellectual curiosity. First and foremost, medical professionals should aim to heal people. After all, they took an oath.


No comments to display.