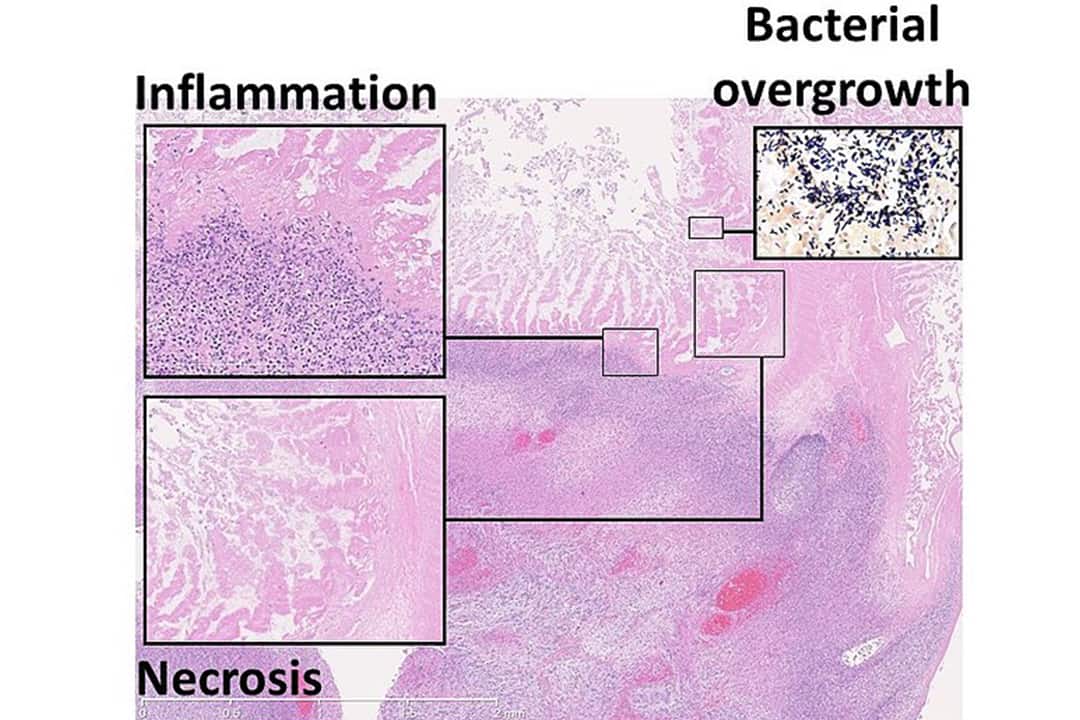
There are a million different things that can go devastatingly wrong in the human body. One of these is the tearing of the intestine, which can sadly occur in infants afflicted with the disease necrotizing enterocolitis. The pathology of this disease is inflammation, which leads to bacterial invasion, which might eventually result in tissue damage. The disease is particularly common in premature infants.
In 1996, Silvia Rudloff and colleagues at the Research Institute of Child Nutrition in Germany first showed that a type of sugar molecule — called human milk oligosaccharides (HMOs) — found in human breast milk appears in the excretions of preterm breast-fed infants but not in formula-fed infants. Further, there’s evidence from a 2012 study to show that HMOs protect neonatal rats against necrotizing enterocolitis.
Building on this research, scientists at U of T recently asked the question: could HMOs be positively impacting babies’ intestines because of the way they affect microorganisms living in the gut? Interestingly, they found that HMOs themselves, independently of these microorganisms, promote intestinal regeneration during necrotizing enterocolitis.
About the intestine
The cells of our intestinal lining are constantly being replaced, with a turnover of only two to five days. Zooming into the lining reveals a fascinating cascade of events that make it possible for us to eat, digest our food, and, ultimately, survive.
Tiny structures called villi stick up from the lining, creating a forest of small protrusions that increase the surface area over which digestion, absorption, and secretion of enzymes can occur. There are also small pockets inside the lining called crypts, in which intestinal stem cells — the source of all the cells that line our guts — lie, awaiting activation.
Like children who don’t yet know what career path they’ll choose, these stem cells are unspecialized. But as they move out of the pocket-like crypts and onto the lining and villi, they specialize into more specific cell types. In normal conditions, these stem cells maintain and regenerate our intestinal lining and ensure that the lining remains healthy.
HMOs promote intestinal regeneration
Returning to the sugar molecules: in 2020, researchers at U of T, The Hospital for Sick Children (SickKids) in Canada, Children’s Hospital of Fudan University in China, and Linköping University in Sweden, using mouse models with necrotizing enterocolitis, found that HMOs promote the specialization of stem cells in intestinal crypts, likely strengthening the gut’s lining through regeneration. But the researchers weren’t done.
A hot topic in the world of medicine is the study of gut microbiota. When people say we aren’t alone in this world, they often refer to aliens — but it applies to our bodies, too. Our intestines are full of friendly creatures, such as bacteria and other microorganisms, that are critical to our health. Scientists now think several diseases, such as inflammatory bowel disease, are linked to abnormal changes in the microbiota.
With this in mind, in a 2024 study published in Pediatric Surgery International, researchers at U of T, SickKids, and McMaster University looked at whether HMOs’ beneficial impact on the intestines of mice with necrotizing enterocolitis is mediated because of the way HMOs change gut microbiota.
To study this, the researchers reduced the amount of intestinal microbiota of pregnant mice using broad-spectrum antibiotics, thereby also affecting the microbiota of their offspring. The mouse pups with disturbed microbiota recovered just as well from the disease as mice with microbiota that had not been changed. All of the offspring in the group who had the disease, who had reduced microbiota, and to whom scientists had administered HMOs had no injuries related to necrotizing enterocolitis. All of this suggests that, unlike what the scientists hypothesized, HMOs don’t act by altering microbiota.
So, the hunt continues. Much remains unknown about these fascinating sugar molecules. But scientists are inching closer and closer to a full picture of the role of HMOs in regenerating intestinal lining. Previous research has already prompted companies to include HMOs in formula milk; perhaps future research will once again change baby formula and take us a step closer to eliminating this devastating disease.


No comments to display.