Freud, who I’d absolutely be down for in another place and time, famously said that clitoral orgasms were infantile and their recipients frigid. Well, pass the mittens, Sigmund.
Like the majority of histories about female health, the story of the clitoris isn’t heartening.
Understandings of the clitoris have largely been shaped by societal norms around femininity, rather than scientific rigour or reality.
Premodern, modern, and even contemporary discourses surrounding the clit are guided mainly by patriarchal priorities. Past depictions of it involved associations with witchcraft, names such as “shameful member,” and claims that the clitoris was effectively a “female penis.”
Disgusted as I may be by the rise of white women calling themselves ‘witches’ for owning a succulent and the like, I do appreciate the associative power of drawing a connection between the clitoris and the supernatural.
In the twentieth century, the clitoris was erased from medical textbooks, including the famous 1948 edition of Gray’s Anatomy, or mentioned with little information and accuracy. For authors and researchers, the clitoris seemed to be a low priority — especially compared to male genitalia, which usually received extensive, accurate coverage. Today, however, this is not necessarily the case.
U of T Associate Professor of Obstetrics and Gynecology Christine Derzko explained that there are a significant number of studies and academic papers dedicated to sexual dysfunction.
But, in her opinion, a “lack of information or misinformation about women’s sexual health has left many women to simply accept sexual difficulties.” This means that women are often suffering in silence “rather than seeking medical help for their problems.” These could include painful intercourse and hypoactive sexual desire disorder, which could be due to psychological issues like emotional or physical abuse. Only relatively recently, in 1981, was an anatomically correct image of the clitoris developed by the Federation of Feminist Women’s Health Clinics. In 2009, the first 3D sonogram of the clitoris was created in France — a famously sexy country — by two researchers in the urology department of Saint-Germain-en-Laye Hospital.
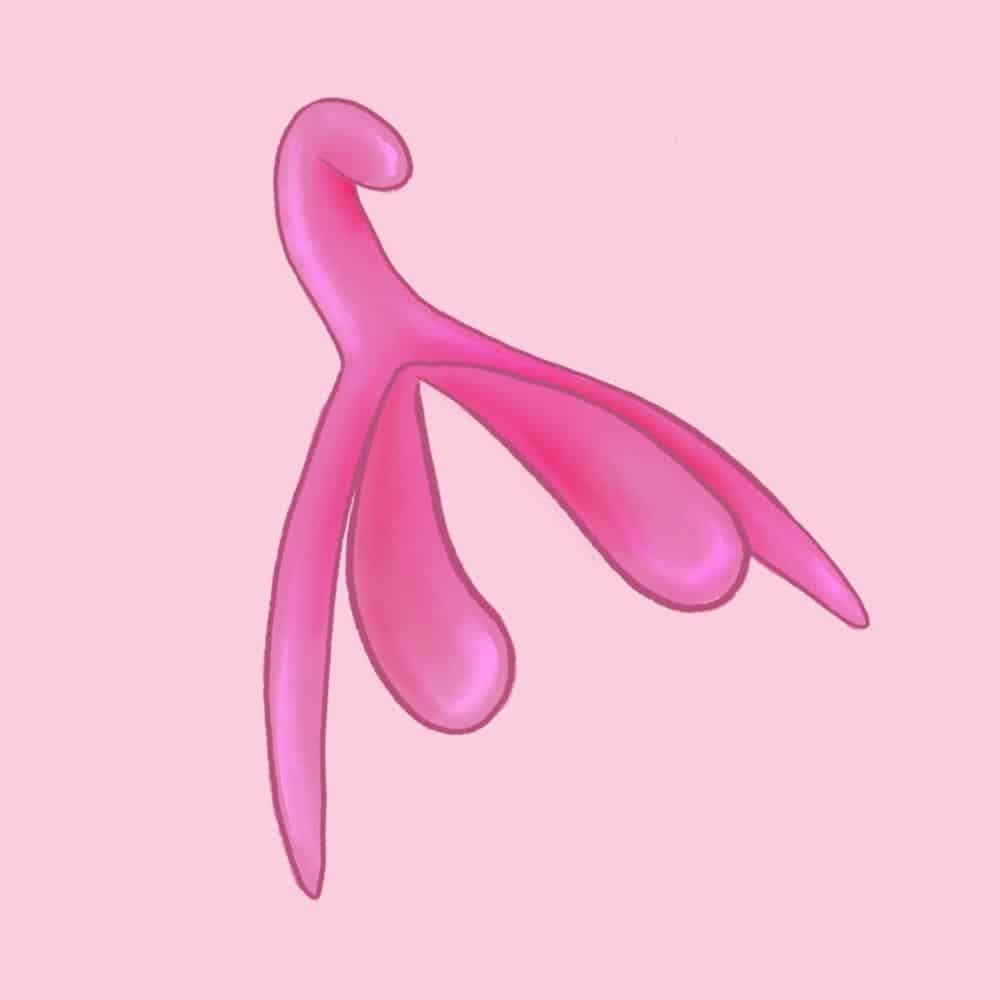
In 2017, French engineer, sociologist, and independent researcher Odile Fillod developed and shared a 3D, life-size model of the clitoris. Contrary to popular belief, the clitoris is not the size of a fingernail!
As Fillod’s model shows, it’s usually over 10 centimetres in size and shaped like a wishbone that would fit nicely in a short person’s palm. Her model is free to download online, and inquiring minds can even print it out for themselves using a 3D printer.
Fillod told The Atlantic that she created the model to help educate young people, who are often taught “that boys are more focused on genital sexuality, whereas girls care more about love and the quality of relationships, in part because of their ‘specific anatomical-physiological characteristics.’”
Although teaching scientifically accurate anatomy doesn’t seem that revolutionary, in this case, it is. Undoing heteronormative, sexist, and essentializing beliefs about traditionally female genitalia is a radical act. Asserting a right to pleasure is political.
The clitoris itself is a bundle of super sensitive nerves above the vagina that extends into the body. It has twice the number of nerve endings as a penis, but, like the penis, has erectile tissue that can swell when stimulated. The clit has great blood supply, which means it can fluctuate in size repeatedly, allowing for multiple orgasms in close succession.
Freud’s argument, first made over 100 years ago, was that as girls matured, they transitioned from clitoral arousal to vaginal. He posited that women who orgasmed from vaginal stimulation were more psychologically mature, competent, and healthy. Although debunked, this theory still resonates today and stigmatizes those who rarely or never orgasm from purely vaginal intercourse.
But, according to a National Institutes of Health (NIH) report, only around 25 per cent of women “always have orgasm from intercourse, while a narrow majority of women have orgasm with intercourse more than half the time” and “roughly one third of women rarely or never have orgasm from intercourse.”
Not only does this Freudian make-believe obscure interest in or care for the clitoris during intercourse, it also unnecessarily segments sexual pleasure between the vagina and the clitoris. Pushing back on this narrative and others that have cropped up to support it is key.
People with different genitalia often experience sexual pleasure differently. While people with penises reliably climax during intercourse, those without usually require different kinds of stimulation. That stimulation varies widely between individuals, making ‘good sex’ much harder to quantify or enumerate.
As explained by the NIH, some “reach orgasm from direct clitoral stimulation, indirect clitoral stimulation, vaginal stimulation or stimulation of internal areas surrounding the vagina,” whereas others orgasm solely from penetrative intercourse, simultaneous stimulation, or not at all.
Derzko explained that while male orgasm is achieved with “a delicate balance between the sympathetic and parasympathetic nervous system,” for females “the experience of orgasm is more complicated.” She highlighted that while “the autonomic nervous system plays an important role, including modulating brainstem function… the stress may lie more heavily on the physical anatomy itself.”
But understanding the clitoris isn’t just important for sexual education — it’s vital for doctors, too. In a 2005 study in the Journal of Urology, researchers reported that “because surgery is guided by accurate anatomy, the quality and validity of available anatomical description are relevant to urologists, gynecologists and other pelvic surgeons.”
This impacts clitoral preservation in invasive surgeries, as well as for broader basic complaints that women might bring to their doctors regarding clitoral pain or infection. On a broader scale, women’s health issues are often misdiagnosed or ignored entirely. Take endometriosis, or the condition where uterine tissue grows on other pelvic organs, which is estimated to affect one in 10 Canadian women but takes, on average, eight to nine years to diagnose and receives relatively little research funding.
As a woman with both a clitoris and endometriosis, this was a sad article to write. I know how frustrating it is to have a doctor dismiss you, or a sexual partner not really grasp your anatomic reality.
This is why better education is necessary for everyone. Fillod’s model is a step in the right direction, but much more needs to be done. We have centuries of misconception to dismiss and so much more to discover.