Parkinson’s disease (PD) is a widely recognized disorder of the nervous system that develops when neurons in the brain die or become damaged.
Some symptoms of this disease include tremors, body stiffness, decreased mobility, and impaired balance and coordination. It affects approximately two per cent of adults over 65 years old and affects men about 1.5 times as frequently as women.
A recent literature review published by researchers at UTSC aims to explain the role of mitochondrial function — or rather dysfunction — as it relates to Parkinson’s disease.
What do mitochondria do?
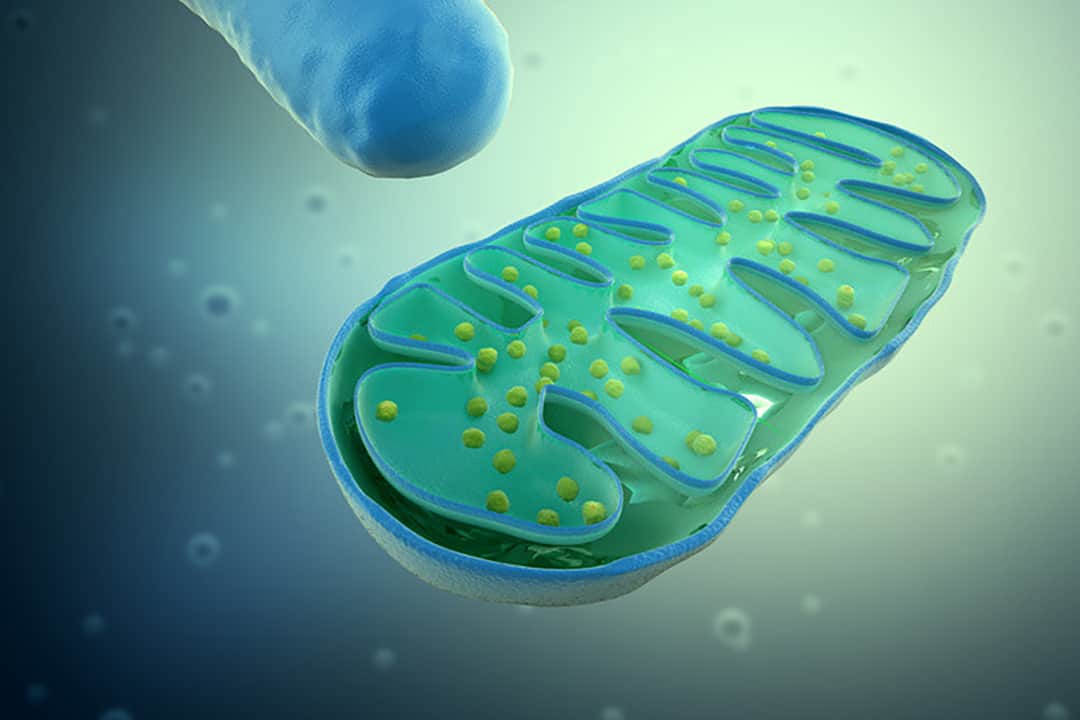
Mitochondria are the cell organelles responsible for generating chemical energy for the body. They also regulate ions in the body and are essential to the well-being of neurons. An oft-quoted internet meme is to refer to them as “powerhouses of the cell,” a common phrase from many high school textbooks that highlights how important they are to the body.
The lead author of the review is PhD candidate Dennison Trinh, a member of the Nash Lab at UTSC. Trinh’s research focuses on the changes in mitochondrial function in rat models of PD.
In his publication, Trinh describes how PD was first linked to mitochondrial dysfunction in the early 1980s, when heroin addicts experienced PD-like symptoms after inadvertently taking heroin laced with a substance called MPTP.
Researchers hypothesized that the mechanisms behind MPTP-induced neurodegeneration might be similar to those that cause PD.
PD and mitochondria
Postmortem studies performed on the brains of patients with PD have shown the impairment of their mitochondria.
Together, these conditions have been shown to compromise the function of mitochondrial DNA, the formation of proteins and lipids, and the regular functioning of associated pathways for biochemical reactions.
Mitochondrial dysfunction was also shown to have been caused by a rise in membrane permeability to calcium. The excess calcium impairs mitochondrial function, sometimes resulting in cell death.
A genetic component
Currently, about five to 10 per cent of PD cases have been linked to genetic mutations, many of which impact mitochondrial function directly or indirectly.
Take the Parkin enzyme for example, which plays an important role in mitochondrial quality control. More than 100 mutations of this enzyme have been linked to PD. These mutations negatively affect Parkin’s enzyme function, preventing the removal of damaged mitochondria.
Evidence also shows that Parkin directly regulates the immune response and that damaged mitochondria are unable to induce an immune response. So Parkin mutations could be triggering the dysregulation of the immune response in patients with PD.
Over 90 additional genetic variants have been identified, which may eventually be used to predict a person’s risk of developing sporadic PD.
Analyses of the different gene variants may indicate not only susceptibility to PD, but also disease progression. However, for now, Trinh wrote that “the best predictor of a person’s likelihood to be diagnosed with PD is their family history of the disease.” And yet, Trinh wrote that a family history of PD “only increases the risk from 1-2% to 3%.” Presently, it is very difficult to accurately predict a person’s predisposition to PD.
Mitochondrial enhancers
Mitochondrial enhancers, therapies that boost mitochondrial function, are being seriously considered in the battle against PD. Preclinical trials have demonstrated the success of some enhancers.
One such mitochondrial enhancer is idebenone, which has shown to alleviate PD-like symptoms and lengthen the lifespan of mouse subjects.
“Since familial and sporadic forms of PD both involve mitochondrial dysfunction at the center of the pathology, we do believe mitochondrial enhancers are key therapeutic agents for treating the disease,” Trinh wrote.
Trinh wrote that “by maintaining or restoring mitochondrial function, the affected neurons should be able to avoid cell death and remain healthy.” Additionally, improvements in the penetration of the blood-brain barrier are likely to facilitate the delivery of mitochondrial enhancers. With so many clinical trials already analyzing treatments for PD, Trinh predicts that a clinical therapeutic could be available within the next five years.
“The greatest takeaway from this review is that PD is a complex disease with many causes, but regardless of cause, central to its pathology is the dysfunction of mitochondria,” Trinh wrote. He goes on to say that in order to develop effective new therapies to combat this disease, “we need to further our understanding of mitochondrial signaling pathways in PD and how to modulate them.”