In 1970, neurosurgeon Dr. Robert White and his colleagues transplanted a monkey’s head onto another monkey’s body. A few years after this experimental breakthrough, he wrote: “What has been accomplished in the animal model… is fully accomplishable in the human sphere. Whether such dramatic procedures will ever be justified in the human area must wait not only upon the continued advance of medical science but more appropriately, the moral and social justification of such procedural undertakings.”
And indeed, in 2017, Dr. Sergio Canavero and Dr. Xiaoping Ren completed the first successful human head transplant between cadavers.
From hypothetical to HEAVEN
Human cephalosomatic anastomosis — the surgical transfer of a head onto a beheaded body under induced hypothermic conditions — hasn’t yet been realized for many reasons, primarily the surgical complication of the procedure of fusing the spinal cords of the head and body of two different individuals to restore motor function.
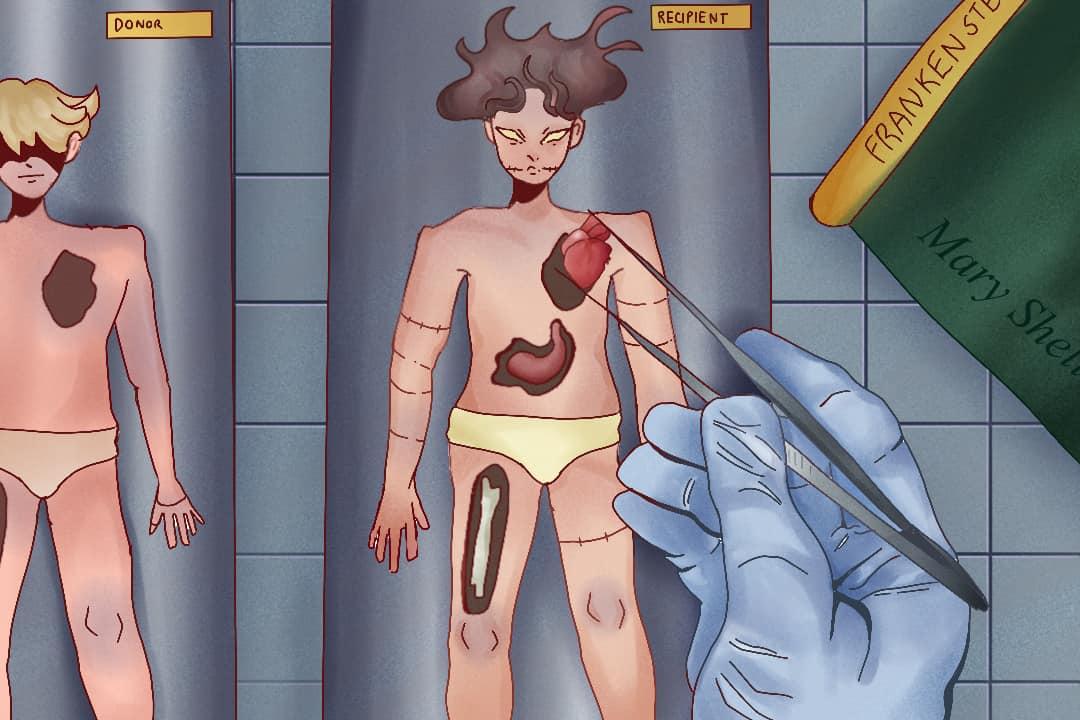
Canavero’s ambition with the human head transplant project takes an interesting lineage. In both 2013 and 2015, Canavero published papers outlining the experimental conditions of a human surgical head transplant — a project he called HEAVEN, short for head anastomosis venture. In the papers, he addressed the principal mechanistic concern about head transplants by designing a spinal cord fusion protocol called project GEMINI, in which polyethylene glycol is used as a fusogen, encouraging cells to fuse. Canavero’s HEAVEN transplant protocol proposes that the patient who has no chance of recovery from injury or disease has their head detached from their body and joined to a brain-dead donor whose body is young and healthy.
In 2015, scientists Anto Čartolovni and Antonio G. Spagnolo raised ethical questions regarding human head transplantation, posing questions about the necessity of a treatment that serves no real therapeutic purpose and only exists to prolong life. Although Canavero proposed in his 2015 paper that the donor and recipient should match in build and immunotype and be screened for systemic disorders, immune rejection still remains a concern.
Čartolovni and Spagnolo believe that the HEAVEN patient would still need regular immunosuppression treatments — drugs that suppress their immune system — so that their body doesn’t reject the transplant. But not only might immunosuppressive therapy be ineffective in eliminating the rejection issue, these drugs also simultaneously compromise the recipient’s tolerance to pathogens that healthy, unsuppressed immune systems would normally withstand.
From a psychological standpoint, Čartolovni and Spagnolo proposed that transplanting a head will also be something of a personality transplant. Modern cognitive science regards the body as a significant part of an individual’s sense of self. The patient with a new body can then have ideas of their former body’s capacities, learned skills, and physiological bounds, which will be obsolete in their new body.
As a result, the patient’s identity may become fragmented, and they will not be able to trust their muscle memory because some of it is irrelevant in its application to their new body. So the chimeric patient may encounter a huge difficulty reconciling their new physical identity.
There’s also the argument that a head transplant might steer people away from donating their organs. In a trolley-problem-like ethical argument, physicians may ask whether the donor’s body should be used to save or prolong one life via the HEAVEN protocol or if it would be more useful by saving multiple patients in line for organ transplants? This is particularly significant to consider in light of Canavero’s true goal of life extension via brain transplants, such that our brains continue in more youthful bodies.
Another ethical standpoint that Canavero tangentially addresses is that the HEAVEN chimera patient would carry the body donor’s gonads — the primary reproductive organs — the transplantation of which several countries prohibit. In this case, after the donor dies, their gonads would live elsewhere and their genetic material would continue to be transmitted by the HEAVEN chimera, inherited by the donor’s biological children and grandchildren who will be born long after the parent dies.
The HEAVEN chimera is not the biological parent of these children; they might not even share the same race. If you have ever wondered about the possibility of someone continuing their genetic line after they have died, consider this prospect.
In 1999, Robert White prophetically and ambitiously wrote, “What has always been the stuff of science fiction — the Frankenstein legend, in which an entire human being is constructed by sewing various body parts together — will become a clinical reality early in the 21st century… brain transplantation, at least initially, will really be head transplantation… With the significant improvements in surgical techniques and postoperative management since then, it is now possible to consider adapting the head-transplant technique to humans.”
A brief history of limb & face transplants
In Ecuador in 1964, doctors performed the first hand transplant, which the recipient’s body immunologically rejected two weeks post-surgery. In 1998, Dr. Jean-Michel Dubernard, surgeon Earl Owen, and the rest of their team carried out the first successful hand transplant in France. However, the patient stopped his immunosuppressive treatments, resulting in tissue rejection and eventual amputation of the hand in 2001. A hand transplant done in 1999 has lasted for at least 20 years. In 2016, 18 surgeons worked for 14 hours, and completed a successful forearm transplant on a live 49-year-old female patient in Toronto that remains successful today!
In 2005, Isabelle Dinoire was the recipient of the first face transplant, which Dubernard’s team carried out. Since then, 47 face transplants have been carried out by 2020, although donation is rare.
Fabricating organs with embryonic stem cells
Grown in the lab, organoids are mini organs with similar architectures and functions as real organs in live humans, but they lack connectivity or biological context, which limits their maturation. The initiating cells of these organoids are derived from human embryonic stem cells. Found in the lining of an early-stage embryo, embryonic stem cells have the potential to become any cell type in the body — a key feature that permits their use in regenerating tissues or even full organs.
It is easy to see, then, the ethical baggage that comes with creating organoids in the lab. Because human embryonic stem cell research often involves the destruction of live human embryos, the discourse regarding stem cell research is closely linked in political content to debates over abortion.
We have yet to see organoid transplants in humans. Such transplants have only been done in animal models, which is a testament to the caution with which this field is approached.
The purpose of these advances should always be to first help victims who have been incapacitated by traumatic injuries or diseases and to improve the efficiency of these procedures. Although donation limits the progression of transplantation, there is greater efficiency in the prospect of organoid transplants. Since there is significant pushback in organoid transplantation due to the political weight of stem cell research, it has not progressed to the point of application to humans. But scientists are ambitious — take Dr. Victor Frankenstein, for example.